Comprehensive Report on Cholangiocarcinoma
1. Overview
What is Cholangiocarcinoma?
Cholangiocarcinoma (CCA) is a rare, aggressive malignancy originating from the epithelial cells of the bile ducts. It represents the second most common primary hepatic malignancy after hepatocellular carcinoma, accounting for approximately 3% of all gastrointestinal cancers. This malignancy is characterized by its insidious onset, late clinical presentation, and poor prognosis.
Affected Body Parts/Organs
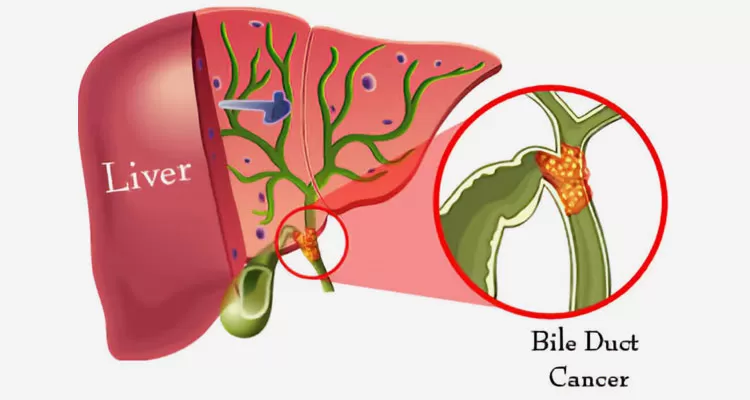
Cholangiocarcinoma affects the biliary tract system, specifically the bile ducts that transport bile from the liver to the small intestine. Based on anatomical location, CCA is classified into three distinct types:
Intrahepatic Cholangiocarcinoma (iCCA): Originates within the liver parenchyma, in the small bile ducts beyond the second-order branches of the left and right hepatic ducts. Accounts for approximately 10-20% of all CCAs.
Perihilar Cholangiocarcinoma (pCCA): Also known as Klatskin tumor, develops at the hepatic duct bifurcation or in the right or left hepatic ducts. Represents about 50-60% of all CCAs and is the most common form.
Distal Cholangiocarcinoma (dCCA): Arises in the common bile duct portion between the cystic duct origin and the ampulla of Vater. Constitutes 20-30% of all CCAs.
Each subtype exhibits distinct epidemiological, clinical, and biological characteristics, requiring different management approaches.
Prevalence and Significance
Cholangiocarcinoma is relatively rare globally, with an annual incidence of 0.5-3.4 per 100,000 persons in Western countries. However, there are remarkable geographical variations:
- High prevalence regions: In Northeast Thailand, where liver fluke infections are endemic, incidence rates reach 85 per 100,000.
- Global trend: The worldwide incidence and mortality rates of CCA, particularly iCCA, have been steadily increasing over the past four decades.
- Significance: Despite its relative rarity, CCA poses significant medical challenges due to its aggressive nature, late diagnosis, limited treatment options, and poor survival rates. The 5-year survival rate ranges from 5-30% depending on the stage at diagnosis.
CCA represents a substantial healthcare burden due to its complex management requirements, high mortality, and rising incidence, particularly in developed countries where risk factors such as obesity, diabetes, and chronic liver disease are becoming more prevalent.
2. History & Discoveries
First Identification
Cholangiocarcinoma was first described as a distinct entity in 1840 by Durand-Fardel, who documented a case of “cancer of the bile ducts.” However, comprehensive understanding of the disease remained limited until the early 20th century.
Key Discoveries and Contributors
The historical development of cholangiocarcinoma knowledge has progressed through several key milestones:
Early descriptions (1840-1900): Following Durand-Fardel’s initial description, isolated case reports appeared in medical literature, but without systematic classification.
Klatskin’s contribution (1965): Gerald Klatskin published his seminal paper describing a specific type of hilar cholangiocarcinoma, which later became known as “Klatskin tumor.” His detailed clinical and pathological characterization significantly advanced understanding of perihilar cholangiocarcinoma.
Liver fluke connection (1950s-1970s): Researchers in Southeast Asia, particularly Thailand, established the causal relationship between liver fluke infections (Opisthorchis viverrini and Clonorchis sinensis) and cholangiocarcinoma, leading to the recognition of one of the first parasite-induced human cancers.
Classification systems (1970s-1990s): Various anatomical classification systems emerged, including:
- The Bismuth-Corlette classification for hilar cholangiocarcinoma (1975)
- The TNM staging system adaptations for cholangiocarcinoma
- The Blumgart classification for surgical planning
Molecular understanding (1990s-2010s): Advances in molecular biology techniques enabled the identification of key genetic alterations in cholangiocarcinoma, including:
- IDH1/2 mutations
- FGFR2 fusions
- BAP1 and ARID1A mutations
- KRAS, BRAF, and TP53 alterations
Evolution of Medical Understanding
Understanding of cholangiocarcinoma has evolved dramatically:
From rare curiosity to established entity: Initially considered an extraordinary malignancy, cholangiocarcinoma is now recognized as an important and increasing cause of liver cancer mortality.
Reclassification efforts: In 2007, the World Health Organization officially recognized intrahepatic cholangiocarcinoma as a distinct entity from hepatocellular carcinoma, addressing previous inconsistencies in classification.
Risk factor identification: Beyond liver flukes, modern epidemiological studies identified various risk factors including primary sclerosing cholangitis, hepatolithiasis, biliary tract anomalies, and chronic viral hepatitis.
Molecular subtyping: Recent research has shifted toward molecular classification, identifying distinct subtypes with different prognoses and potential therapeutic vulnerabilities:
- Proliferation subtype (worse prognosis)
- Inflammation subtype (better prognosis)
- Metabolism subtype
Multidisciplinary approach: Recognition that optimal management requires collaboration between hepatobiliary surgeons, medical oncologists, radiation oncologists, interventional radiologists, and palliative care specialists.
This evolution reflects the transition from purely descriptive approaches to sophisticated molecular characterization, enabling more personalized treatment strategies for patients with cholangiocarcinoma.
3. Symptoms
Cholangiocarcinoma typically presents with non-specific symptoms that often appear only in advanced stages, contributing to delayed diagnosis and poor outcomes.
Early Symptoms
Early-stage cholangiocarcinoma is frequently asymptomatic or presents with vague manifestations that are easily attributed to other conditions:
- Fatigue and malaise: Often the earliest symptoms, but frequently overlooked
- Mild abdominal discomfort: Vague, intermittent right upper quadrant or epigastric pain
- Unexplained weight loss: Gradual and often unnoticed initially
- Low-grade fever: Occasionally present, especially with inflammation or infection
- Early satiety: Feeling full after eating small amounts
- Mild pruritus (itching): May occur before jaundice becomes apparent
These subtle manifestations often result in diagnostic delays averaging 4-6 months from symptom onset to diagnosis.
Advanced-Stage Symptoms
As the disease progresses, more specific and severe symptoms emerge:
Jaundice: Yellowing of skin and sclera due to biliary obstruction
- Present in 90% of perihilar and distal cholangiocarcinomas
- Less common in intrahepatic cholangiocarcinomas (10-30%)
- Often painless when occurring in isolation
Cholangitis: Inflammation of bile ducts presenting as:
- High fever with chills
- Right upper quadrant pain
- Worsening jaundice (Charcot’s triad)
- Potentially life-threatening condition requiring urgent intervention
Abdominal pain: Becomes more localized and severe
- Right upper quadrant or epigastric region
- May radiate to the back
- Often dull and persistent
Cachexia: Severe weight loss and muscle wasting from cancer-related metabolism changes
Hepatomegaly: Enlarged liver detected on physical examination
Ascites: Accumulation of fluid in the peritoneal cavity, indicating advanced disease
Clay-colored stools and dark urine: Due to biliary obstruction and bilirubin redirection
Common vs. Rare Symptoms
Common symptoms (present in >30% of patients):
- Jaundice (60-80% overall)
- Weight loss (30-50%)
- Abdominal pain (30-40%)
- Fatigue (20-35%)
- Pruritus (20-25%)
- Fever (20%)
Rare symptoms (<10% of patients):
- Palpable gallbladder (Courvoisier’s sign, 5-10%)
- Migratory thrombophlebitis (Trousseau’s syndrome, 3-5%)
- Gastrointestinal bleeding (1-5%)
- Hemobilia (blood in bile, <1%)
- Paraneoplastic syndromes (e.g., dermatomyositis, <1%)
Symptom Progression
The typical progression pattern follows this timeline:
Initial phase (months 0-3):
- Nonspecific fatigue, malaise
- Subtle weight loss
- Vague abdominal discomfort
Intermediate phase (months 3-6):
- Increasing abdominal pain
- Noticeable weight loss
- Onset of jaundice in obstructive cases
Advanced phase (months 6+):
- Persistent, severe jaundice
- Significant weight loss and cachexia
- Fever and signs of infection
- Ascites, hepatomegaly, and potential portal hypertension
- Symptoms of metastatic disease (bone pain, dyspnea, neurological symptoms)
Symptom presentation varies significantly by anatomical subtype:
- Intrahepatic CCA: Often presents late with nonspecific symptoms; jaundice is less common
- Perihilar CCA: Typically presents with progressive jaundice as the first sign
- Distal CCA: Presents with jaundice, often accompanied by pruritus and abdominal pain
The insidious nature of symptom onset and progression contributes significantly to the typically advanced stage at diagnosis, with approximately 70% of patients presenting with unresectable or metastatic disease.
4. Causes
Biological Causes
At the cellular and molecular level, cholangiocarcinoma arises from a complex interplay of genetic alterations and dysregulated cellular pathways:
Genetic Mutations:
- IDH1/2 mutations: Present in 10-20% of intrahepatic CCAs, leading to altered cellular metabolism and epigenetic dysregulation
- FGFR2 fusions/rearrangements: Found in 10-15% of intrahepatic CCAs, causing constitutive activation of growth factor signaling
- KRAS mutations: Common in all subtypes (15-25%), activating downstream proliferative pathways
- TP53 mutations: Present in 20-40% of cases, compromising DNA damage response and apoptosis
- CDKN2A/B inactivation: Found in 20-30% of cases, disrupting cell cycle regulation
- ARID1A mutations: Occur in 15-20% of cases, affecting chromatin remodeling
- BAP1 mutations: Present in 10-15% of intrahepatic CCAs, affecting DNA repair mechanisms
Dysregulated Signaling Pathways:
- Notch pathway activation: Promotes cholangiocyte differentiation and proliferation
- IL-6/STAT3 signaling: Drives inflammation-associated carcinogenesis
- WNT/β-catenin pathway: Influences cellular proliferation and invasion
- TGF-β pathway: Contributes to epithelial-mesenchymal transition and metastasis
- EGFR/HER2 signaling: Promotes cellular proliferation and survival
Cellular Processes:
- Chronic inflammation: Causes DNA damage through reactive oxygen species
- Biliary epithelial-to-mesenchymal transition: Enhances cellular invasiveness
- Aberrant cell cycle regulation: Allows uncontrolled proliferation
- Impaired DNA repair mechanisms: Leads to genomic instability
- Altered bile acid metabolism: Creates toxic microenvironment
Environmental Causes
Environmental factors play a significant role in cholangiocarcinoma development, particularly in specific geographic regions:
Parasitic Infections:
- Opisthorchis viverrini: Endemic in Thailand, Laos, and Cambodia, increases risk 15-fold
- Clonorchis sinensis: Common in China, Taiwan, Korea, and Vietnam
- Mechanisms: Chronic inflammation, mechanical damage to bile ducts, secretion of carcinogenic proteins
Chemical Carcinogens:
- Thorotrast: Previously used contrast agent, increases risk 300-fold with latency of 16-45 years
- Dioxin exposure: Associated with increased incidence in chemical plant workers
- Vinyl chloride: Occupational exposure linked to bile duct cancer
- Nitrosamines: Present in preserved foods, particularly in high-incidence regions
- Asbestos: Occupational exposure linked to increased risk
Water and Food Contaminants:
- Aflatoxin B1: Fungal contaminant in stored grains and nuts
- Arsenic: Contaminated drinking water in certain regions
- Polycyclic aromatic hydrocarbons: From industrial pollution and cooking practices
Genetic and Hereditary Factors
While most cholangiocarcinoma cases are sporadic, several genetic conditions increase susceptibility:
Hereditary Syndromes:
- Lynch syndrome (hereditary non-polyposis colorectal cancer): 2-4 fold increased risk
- BRCA1/2 mutations: Modestly increased risk, particularly with BRCA2
- Multiple biliary papillomatosis: Rare condition with high malignant transformation risk
- BAP1 tumor predisposition syndrome: Associated with increased intrahepatic CCA risk
Familial Clustering:
- First-degree relatives of CCA patients have 2-3 times higher risk
- Particularly pronounced in regions with high baseline risk
Genetic Polymorphisms:
- Variations in genes involved in bile acid metabolism (e.g., ABCB11, ABCB4)
- Polymorphisms in inflammatory response genes (e.g., IL6, TNF-α)
- Variations in carcinogen-metabolizing enzymes (e.g., GST, NAT2)
Known Triggers
Several established triggers can precipitate cholangiocarcinoma development, particularly in susceptible individuals:
Biliary Tract Abnormalities:
- Choledochal cysts: 10-15% lifetime risk of malignant transformation
- Hepatolithiasis: Intrahepatic stones, common in East Asia
- Caroli disease: Congenital cystic dilatation of intrahepatic bile ducts
- Biliary-enteric anastomosis: Creates ascending bacterial colonization
- Cholelithiasis: Gallstones modestly increase risk (1.5-2 fold)
Inflammatory Conditions:
- Primary sclerosing cholangitis (PSC): Highest risk factor in Western populations (5-15% lifetime risk)
- Chronic typhoid carriage: Particularly Salmonella typhi, acts as cofactor
- Recurrent pyogenic cholangitis: Common in Southeast Asia
- Hepatitis B and C: 2-4 fold increased risk, more pronounced with cirrhosis
- Nonalcoholic steatohepatitis: Emerging risk factor with rising incidence
Metabolic Disorders:
- Type 2 diabetes mellitus: 1.5-2 fold increased risk
- Obesity: Independent risk factor, particularly for intrahepatic CCA
- Nonalcoholic fatty liver disease: Increasingly recognized risk factor
The multifactorial etiology of cholangiocarcinoma explains its geographical variations and the diverse molecular profiles observed in different populations, underscoring the need for region-specific prevention strategies and personalized therapeutic approaches.
5. Risk Factors
Demographic Factors
Age
- Peak incidence: 50-70 years
- Median age at diagnosis: 67 years in Western countries, 50-60 years in endemic regions
- Age-related risk: Incidence increases exponentially after age 40
- Juvenile cases: Extremely rare (<1%) and often associated with congenital biliary abnormalities
Gender
- Overall ratio: Slight male predominance (male-to-female ratio approximately 1.2-1.5:1)
- Variation by subtype:
- Intrahepatic CCA: Stronger male predominance (1.5-2:1)
- Extrahepatic CCA: More equal distribution (1.1-1.3:1)
- Hormonal factors: Limited evidence for estrogen as potential protective factor
Ethnicity and Geography
- Highest incidence: Northeast Thailand (85/100,000), northern China, South Korea
- Intermediate incidence: Japan, Singapore, Eastern Europe
- Lowest incidence: North America, Western Europe, Australia (0.5-3/100,000)
- Indigenous populations: Higher rates among Native Americans and Alaska Natives
- Hispanic populations: Higher rates compared to non-Hispanic whites in the US
- Asian Americans: Higher rates compared to other American ethnic groups
Medical Conditions
Primary Sclerosing Cholangitis (PSC)
- Risk magnitude: 400-1000 fold increased risk
- Lifetime risk: 5-15% of PSC patients develop CCA
- Characteristics: Often occurs early in PSC course, difficult to detect
- Median survival after diagnosis: 5-7 months
- Screening: Challenging but recommended with CA19-9, imaging
Liver Diseases
- Viral hepatitis:
- Hepatitis B: 2.5-5 fold increased risk
- Hepatitis C: 2-4 fold increased risk
- Mechanism: Chronic inflammation, cirrhosis development
- Cirrhosis: 5-10 fold increased risk, regardless of etiology
- Nonalcoholic fatty liver disease (NAFLD):
- 2-3 fold increased risk
- Rapidly increasing contributor in Western countries
- Alcoholic liver disease: 2-3 fold increased risk
Biliary Tract Conditions
- Choledochal cysts: 10-15% lifetime risk
- Hepatolithiasis: 5-7% of affected patients develop CCA
- Biliary papillomatosis: Up to 40% malignant transformation
- Thorotrast exposure: 300-fold increased risk
- Bile duct adenoma: Potential precursor lesion
Inflammatory Bowel Disease
- Ulcerative colitis: 2-4 fold increased risk, independent of PSC
- Crohn’s disease: Modest increased risk (1.5-2 fold)
- Duration effect: Risk increases with longer disease duration
Lifestyle and Environmental Factors
Smoking
- Risk magnitude: 1.5-2.5 fold increased risk
- Dose-response: Risk correlates with pack-years
- Synergistic effect: Particularly harmful when combined with other risk factors
- Cessation benefit: Risk gradually decreases after cessation
Alcohol Consumption
- Direct effects: 1.5-2 fold increased risk with heavy consumption (>80g/day)
- Indirect effects: Through development of liver disease
- Gender differences: Possibly stronger association in men
Occupational Exposures
- Chemical workers: Exposure to dioxins, vinyl chloride, formaldehyde
- Printing industry: Exposure to organic solvents
- Rubber manufacturing: Multiple chemical exposures
- Asbestos workers: 4-5 fold increased risk in heavily exposed workers
- Petrochemical workers: Modestly elevated risk
Dietary Factors
- Nitrosamine-rich foods: Preserved fish, processed meats
- Aflatoxin contamination: In regions with poor food storage
- Raw freshwater fish: Vehicle for liver fluke transmission
- Protective factors: Limited evidence for coffee, fruits, vegetables
Genetic and Familial Factors
Inherited Syndromes
- Lynch syndrome: 2-4 fold increased risk
- BRCA1/2 mutations: Modest increased risk
- BAP1 tumor predisposition: Associated with intrahepatic CCA
- Cystic fibrosis: Increased risk through liver and biliary involvement
Family History
- First-degree relatives: 2-3 fold increased risk
- Familial clustering: More pronounced in high-incidence regions
- Multi-generational patterns: Rare but reported
Genetic Polymorphisms
- Inflammatory pathway genes: IL6, TNF-α, TGF-β
- Xenobiotic metabolism: GSTM1, GSTT1, NAT2
- DNA repair genes: XRCC1, OGG1
The complex interplay between these various risk factors explains the geographical and demographic variations in cholangiocarcinoma incidence and supports a multifactorial model of carcinogenesis. This understanding can guide targeted screening of high-risk populations, potentially enabling earlier diagnosis and improving outcomes.
6. Complications
Cholangiocarcinoma leads to numerous complications that significantly impact patient morbidity, mortality, and quality of life. These complications arise from both the primary disease process and its treatments.
Disease-Related Complications
Biliary Obstruction
- Mechanism: Tumor growth within or compressing bile ducts
- Clinical manifestations:
- Jaundice (progressive, often intractable)
- Pruritus (often severe and debilitating)
- Malabsorption of fat-soluble vitamins (A, D, E, K)
- Steatorrhea (fatty, foul-smelling stools)
- Secondary effects:
- Coagulopathy from vitamin K deficiency
- Osteoporosis from vitamin D deficiency
- Night blindness from vitamin A deficiency
Cholangitis
- Incidence: Occurs in 20-30% of patients
- Mechanism: Bacterial colonization of obstructed bile ducts
- Presentation: Fever, right upper quadrant pain, worsening jaundice (Charcot’s triad)
- Severity: Can progress to septic shock (Reynolds’ pentad)
- Mortality: 10-50% if inadequately treated
- Recurrence: Common even after initial management
Liver Dysfunction and Failure
- Mechanisms:
- Progressive biliary obstruction causing secondary biliary cirrhosis
- Direct tumor invasion of functional liver tissue
- Portal vein involvement causing portal hypertension
- Manifestations:
- Hepatomegaly
- Ascites
- Coagulopathy
- Hypoalbuminemia
- Hepatic encephalopathy
- Timeline: May develop over months to years depending on tumor location and growth
Metastatic Spread
- Common sites:
- Regional lymph nodes (50-60% at diagnosis)
- Liver (particularly for distal and perihilar CCA)
- Peritoneum (15-20%)
- Lungs (5-15%)
- Bone (5-10%)
- Manifestations:
- Lymphadenopathy
- Malignant ascites
- Bone pain
- Pathological fractures
- Neurological symptoms with brain metastases (rare)
Vascular Complications
- Portal vein thrombosis/involvement: 15-20% of cases
- Hepatic artery involvement: 10-15% of cases
- Venous thromboembolism: 10-15% incidence, higher with advanced disease
- Budd-Chiari syndrome: Rare but serious complication
Treatment-Related Complications
Surgical Complications
- Perioperative mortality: 5-10% for major hepatectomy with bile duct resection
- Major morbidity: 30-40% of surgical patients
- Specific complications:
- Bile leak (10-15%)
- Post-hepatectomy liver failure (8-10%)
- Intra-abdominal abscess (10-15%)
- Wound infection (15-20%)
- Anastomotic stricture (10-15%)
- Bleeding (5-10%)
Biliary Drainage Complications
- Percutaneous transhepatic biliary drainage (PTBD):
- Hemorrhage (2-5%)
- Bile leak (2%)
- Cholangitis (5-10%)
- Catheter dislodgement (5-7%)
- Endoscopic retrograde cholangiopancreatography (ERCP):
- Pancreatitis (5-10%)
- Stent occlusion (30-40% within 3-4 months)
- Perforation (1%)
- Cholangitis (5%)
Chemotherapy-Related Complications
- Gemcitabine/cisplatin regimen:
- Myelosuppression (30-45%)
- Nausea/vomiting (30-40%)
- Peripheral neuropathy (15-30%)
- Nephrotoxicity (10-20%)
- FOLFOX regimen:
- Peripheral neuropathy (40-50%)
- Diarrhea (30-40%)
- Myelosuppression (20-30%)
Radiation Therapy Complications
- Acute:
- Fatigue (50-60%)
- Nausea (30-40%)
- Skin changes (20-30%)
- Late:
- Radiation-induced liver disease (5-10%)
- Biliary stricture (5-15%)
- Small bowel injury (5-10%)
Long-term Impact on Organs and Health
Hepatobiliary System
- Progressive biliary fibrosis: Even after successful initial treatment
- Secondary biliary cirrhosis: Developing over 1-5 years
- Portal hypertension: With associated varices and bleeding risk
- Recurrent cholangitis: Particularly with biliary stents or anastomoses
Systemic Effects
- Cancer cachexia syndrome:
- Severe weight loss
- Muscle wasting
- Anorexia
- Fatigue
- Malnutrition: Due to combination of reduced intake and malabsorption
- Chronic pain: Requiring long-term pain management
- Psychological impact: Depression, anxiety, fear of recurrence
Mortality and Disability
Mortality Rates
- Overall median survival (untreated): 3-6 months
- Overall median survival (treated): 12-36 months depending on stage
- 5-year survival by stage:
- Stage I: 30-50%
- Stage II: 15-30%
- Stage III: 5-15%
- Stage IV: <5%
- Cause-specific mortality:
- Liver failure (30-40%)
- Infectious complications (20-30%)
- Tumor progression/cachexia (30-40%)
- Treatment-related (5-10%)
Disability and Functional Impact
- Performance status decline: Often rapid with advanced disease
- Activities of daily living: Progressively limited by fatigue, pain, ascites
- Occupational disability: Often complete by advanced stages
- Care dependency: High in advanced stages
The complex interplay of these complications significantly impacts treatment decisions, quality of life, and survival outcomes. Early recognition and proactive management of complications are essential components of comprehensive care for patients with cholangiocarcinoma.
7. Diagnosis & Testing
Early and accurate diagnosis of cholangiocarcinoma remains challenging due to its often vague presenting symptoms and the deep anatomical location of the biliary tract. A systematic approach using multiple diagnostic modalities is typically required.
Clinical Evaluation
History and Physical Examination
- Key history elements:
- Risk factor assessment (PSC, liver fluke exposure, etc.)
- Symptom onset and progression
- Weight loss quantification
- Pruritus severity and timing
- Prior biliary disease
- Physical examination findings:
- Jaundice (scleral, skin)
- Hepatomegaly
- Right upper quadrant tenderness
- Scratch marks from pruritus
- Courvoisier’s sign (palpable, nontender gallbladder)
- Cachexia and muscle wasting
- Ascites
Laboratory Tests
Liver Function Tests
- Pattern in obstruction:
- Elevated bilirubin (predominantly direct/conjugated)
- Elevated alkaline phosphatase (ALP) and gamma-glutamyl transferase (GGT)
- Moderately elevated transaminases (AST, ALT)
- Typical values:
- Bilirubin: 5-20 mg/dL
- ALP: 2-10 times upper limit of normal
- GGT: 5-15 times upper limit of normal
- AST/ALT: 1-3 times upper limit of normal
Tumor Markers
- Carbohydrate antigen 19-9 (CA 19-9):
- Sensitivity: 40-70%
- Specificity: 50-80%
- Limitations: False positives with biliary obstruction, cholangitis
- Not elevated in 10% of population (Lewis antigen negative)
- Most useful for monitoring response to therapy
- Carcinoembryonic antigen (CEA):
- Sensitivity: 30-50%
- Often used in combination with CA 19-9
- Cancer antigen 125 (CA-125):
- Elevated in 40-50% of cases
- Low specificity
- Alpha-fetoprotein (AFP):
- Usually normal in pure CCA
- May be elevated in mixed HCC-CCA
Emerging Biomarkers
- microRNAs: miR-21, miR-221
- Circulating tumor DNA: KRAS, IDH1/2, FGFR2 mutations
- Bile proteomics: S100A8, S100A9, CEAM5, MUC5AC
- Metabolomics: Bile acid profiles
- Exosomal markers: Still investigational
Imaging Studies
Ultrasonography
- Utility: Often first-line imaging
- Findings:
- Bile duct dilatation
- Mass lesion (in some cases)
- Lymphadenopathy
- Limitations: Operator-dependent, limited visualization of distal bile ducts
- Sensitivity: 50-70% overall
- Enhancement: Contrast-enhanced ultrasound improves detection of masses
Computed Tomography (CT)
- Protocol: Triphasic CT with arterial, venous, and delayed phases
- Findings by subtype:
- Intrahepatic CCA: Hypodense mass with peripheral enhancement and delayed central fill-in
- Perihilar CCA: Bile duct thickening, enhancement, and stricture
- Distal CCA: Bile duct wall thickening with enhancement
- Additional value: Assesses vascular invasion, lymph nodes, distant metastases
- Sensitivity: 70-80% overall
- Specificity: 70-80%
Magnetic Resonance Imaging (MRI)
- Protocol: MRI with MRCP (magnetic resonance cholangiopancreatography)
- Findings:
- T1: Hypointense mass
- T2: Variably hyperintense
- Dynamic contrast: Peripheral enhancement with progressive central fill-in
- MRCP advantages:
- Non-invasive biliary mapping
- Visualization of ductal involvement
- Assessment of liver volume
- Sensitivity: 80-90%
- Specificity: 80-85%
Positron Emission Tomography (PET)
- Utility: Limited for primary diagnosis, useful for metastatic evaluation
- Tracer: 18F-fluorodeoxyglucose (FDG)
- Sensitivity: 60-70% overall
- Better for intrahepatic (70-80%)
- Lower for extrahepatic (50-60%)
- Specific use: Detection of distant metastases, recurrence after treatment
Invasive Diagnostic Procedures
Endoscopic Retrograde Cholangiopancreatography (ERCP)
- Utility: Diagnostic and therapeutic
- Findings: Strictures, filling defects, irregularity
- Sampling methods:
- Brush cytology (sensitivity: 30-60%)
- Intraductal biopsy (sensitivity: 40-70%)
- SpyGlass direct visualization with targeted biopsy (sensitivity: 60-80%)
- Advantages: Allows biliary drainage
- Limitations: Risk of pancreatitis (5-10%), primarily useful for distal and perihilar CCA
Percutaneous Transhepatic Cholangiography (PTC)
- Utility: Alternative to ERCP, especially for proximal lesions
- Findings: Similar to ERCP
- Sampling: Percutaneous biopsy possible
- Advantages: Better access to proximal biliary tree
- Limitations: Risk of bleeding, bile leak
Endoscopic Ultrasound (EUS)
- Utility: Evaluation of distal bile duct and regional lymph nodes
- Advantages:
- Fine needle aspiration (FNA) of masses
- High resolution imaging of distal biliary tree
- Sensitivity of EUS-FNA: 70-90%
- Specificity of EUS-FNA: >90%
- Limitations: Less useful for proximal lesions
Tissue Diagnosis
Approaches
- Percutaneous biopsy: For intrahepatic masses
- Endoscopic approaches:
- ERCP with brushing/biopsy
- EUS-guided FNA/FNB (fine needle biopsy)
- Surgical: Occasionally required when other methods inconclusive
Histopathologic Features
- Common features:
- Adenocarcinoma (>90%)
- Varying degrees of differentiation
- Desmoplastic stroma
- Variants:
- Mucinous
- Clear cell
- Squamous
- Sarcomatoid
Immunohistochemistry
- Positive markers:
- CK7 (90-95%)
- CK19 (80-90%)
- MOC31 (70-80%)
- CA19-9 (70-80%)
- Negative markers:
- CK20 (10-20% positive)
- HepPar1 (distinguishes from HCC)
Molecular Testing
- Actionable mutations:
- IDH1/2 mutations
- FGFR2 fusions
- NTRK fusions
- MSI/dMMR status
- BRAF V600E
Staging
TNM Classification
- American Joint Committee on Cancer (AJCC) 8th edition:
- Separate staging systems for intrahepatic, perihilar, and distal CCA
- Based on tumor size, number, vascular invasion, lymph node involvement, distant metastases
- Bismuth-Corlette classification: For perihilar CCA
- Type I: Below confluence
- Type II: At confluence
- Type III: Extends to right (IIIA) or left (IIIB) hepatic duct
- Type IV: Extends to both hepatic ducts
Surgical Staging
- Blumgart staging system: For perihilar CCA
- Assesses biliary extent, portal vein involvement, hepatic lobar atrophy
- Predicts resectability
- Liver remnant volume and function:
- Critical for surgical planning
- Future liver remnant (FLR) >30% required (>40% with cirrhosis)
Early Detection and Screening
High-Risk Population Screening
- PSC patients:
- Annual magnetic resonance imaging/MRCP
- Serum CA 19-9 (with cautious interpretation)
- No proven survival benefit
- Other high-risk groups:
- No established screening protocols
- Areas of endemicity for liver flukes: Periodic ultrasonography proposed
Challenges in Early Detection
- Anatomical location: Deep within the abdomen
- Slow-growing nature: Often asymptomatic until advanced
- Biomarker limitations: Lack of highly sensitive, specific markers
- Cost-effectiveness: Limited by low prevalence in general population
The diagnostic approach to cholangiocarcinoma continues to evolve with improvements in imaging resolution, endoscopic techniques, and molecular diagnostics. A multidisciplinary approach to diagnosis, involving radiologists, endoscopists, pathologists, and surgeons, offers the best chance for accurate and timely diagnosis of this challenging malignancy.
8. Treatment Options
The management of cholangiocarcinoma requires a multidisciplinary approach, with treatment strategies tailored according to disease location, stage, and patient factors. Despite advances, curative options remain limited and are applicable to only a minority of patients.
Surgical Management
Resection
Intrahepatic CCA:
- Procedure: Anatomical hepatectomy with lymphadenectomy
- Margin requirements: R0 resection (negative margins) with 5-10mm minimum
- Lymphadenectomy: Hilar and regional nodes
- Resectability rate: 30-40% of cases
- Operative mortality: 3-5%
- 5-year survival: 20-35%
Perihilar CCA:
- Procedure: Bile duct resection with major hepatectomy and caudate lobectomy
- Extent: Based on Bismuth-Corlette classification
- Vascular resection: Portal vein/hepatic artery reconstruction when necessary
- Resectability rate: 20-30% of cases
- Operative mortality: 5-10%
- 5-year survival: 20-30%
Distal CCA:
- Procedure: Pancreaticoduodenectomy (Whipple procedure)
- Resectability rate: 30-40%
- Operative mortality: 2-5%
- 5-year survival: 20-30%
Contraindications to Resection
- Bilateral, multifocal disease
- Distant metastases
- Major vascular encasement
- Underlying severe liver dysfunction
- Bilateral involvement of sectoral ducts
- Poor performance status
Liver Transplantation
- Mayo Clinic Protocol (for selected perihilar CCA):
- Eligibility: Early-stage, unresectable perihilar CCA, preferably in PSC patients
- Neoadjuvant therapy: External beam radiation + 5-FU followed by brachytherapy
- Results: 5-year survival 65-70% in select centers
- Limitations: Strict selection criteria, limited availability
Non-Surgical Management
Biliary Drainage
- Indications: Biliary obstruction with cholangitis or intractable pruritus
- Endoscopic approaches:
- Metal stents (preferred for malignant obstruction)
- Plastic stents (shorter patency, easier replacement)
- Percutaneous approaches:
- External drainage
- Internal-external drainage
- Metallic stent placement
- Complications: Cholangitis, occlusion, migration
- Palliative benefit: Improved quality of life, prerequisite for chemotherapy
Systemic Therapy
First-Line Treatment
- Standard regimen: Gemcitabine plus cisplatin
- Evidence: ABC-02 trial established standard of care
- Response rate: 26-31%
- Median survival benefit: 11.7 vs 8.1 months compared to gemcitabine alone
- Toxicity: Myelosuppression, nausea, fatigue, nephrotoxicity
- Alternative regimens:
- GEMOX (gemcitabine + oxaliplatin): Similar efficacy, different toxicity profile
- FOLFOX (5-FU, leucovorin, oxaliplatin): Option for patients unfit for gemcitabine
Second-Line Treatment
- FOLFOX: After gemcitabine-based first-line
- FOLFIRI: Irinotecan-based regimen with modest activity
- Clinical trial enrollment: Strongly encouraged
Targeted Therapies
- FGFR inhibitors (for FGFR2 fusion-positive iCCA):
- Pemigatinib: FDA-approved, 35% response rate
- Infigratinib: 23% response rate
- Futibatinib: 42% response rate
- IDH inhibitors (for IDH1-mutated iCCA):
- Ivosidenib: Modest benefit in progression-free survival
- NTRK inhibitors (for NTRK fusion-positive cases):
- Larotrectinib, entrectinib
- BRAF inhibitors (for BRAF V600E-mutated cases):
- Dabrafenib + trametinib
Immunotherapy
- MSI-high/dMMR tumors:
- Pembrolizumab: FDA-approved for MSI-high tumors regardless of origin
- Response rate: 40-50% in this rare subset
- Unselected patients:
- Limited efficacy as monotherapy (5-10% response rate)
- Combination strategies under investigation
Locoregional Therapies
Radiation Therapy
- External beam radiation therapy (EBRT):
- Indications: Adjuvant setting, unresectable disease
- Technique: Intensity-modulated radiation therapy (IMRT) preferred
- Dose: Typically 45-54 Gy in 1.8-2.0 Gy fractions
- Results: Local control benefit, unclear survival impact
- Stereotactic body radiation therapy (SBRT):
- Advantages: Short treatment course, precise delivery
- Applications: Primarily intrahepatic CCA
- Dose: 30-60 Gy in 3-5 fractions
Liver-Directed Therapies
- Transarterial chemoembolization (TACE):
- Indication: Unresectable intrahepatic CCA
- Response rate: 20-30%
- Survival benefit: Modest (3-6 months improvement in selected cases)
- Radioembolization (Y-90):
- Indication: Unresectable intrahepatic CCA
- Advantage: Single session, minimal side effects
- Results: Median survival 15-20 months in selected cases
- Ablative therapies:
- Techniques: Radiofrequency ablation, microwave ablation
- Applications: Small (<3cm) intrahepatic CCA
- Limitations: High local recurrence rates
Multimodal Approaches
Adjuvant Therapy
- BILCAP trial results:
- Capecitabine for 6 months after resection
- Per-protocol analysis showed survival benefit
- Now standard of care in many centers
- Radiation therapy:
- Consider for R1 resection (microscopically positive margins)
- No established survival benefit
- Current recommendations:
- Capecitabine for 6 months after resection
- Consider chemoradiation for high-risk features (positive margins, lymph node involvement)
Neoadjuvant Therapy
- Potential benefits:
- Downsizing borderline resectable disease
- Testing biological behavior before major surgery
- Early treatment of micrometastatic disease
- Approaches:
- Gemcitabine/cisplatin chemotherapy
- Chemoradiation in selected cases
- Evidence base: Limited, primarily institutional series
Palliative and Supportive Care
Symptom Management
- Pruritus control:
- Bile acid sequestrants (cholestyramine)
- Antihistamines
- Rifampicin
- Opioid antagonists
- Sertraline
- Pain management:
- Multimodal approach
- Celiac plexus block for refractory pain
- Nutritional support:
- Medium-chain triglyceride supplements
- Fat-soluble vitamin replacement
- Enteral feeding as needed
End-of-Life Care
- Early palliative care consultation: Associated with improved quality of life
- Advance care planning: Recommended at diagnosis of advanced disease
- Hospice referral: Consider when performance status declining or after failure of second-line therapy
Emerging Treatments and Clinical Trials
Novel Targeted Approaches
- Fibroblast growth factor receptor (FGFR) inhibitors: Newer generations with improved toxicity profiles
- RAS pathway inhibitors: MEK inhibitors, TRK inhibitors
- Epigenetic modulators: HDAC inhibitors, BET inhibitors
- Cell cycle inhibitors: CDK4/6 inhibitors
Immunotherapy Advances
- Combination approaches:
- Dual checkpoint blockade (anti-PD-1/PD-L1 + anti-CTLA-4)
- Checkpoint inhibitors + targeted therapy
- Checkpoint inhibitors + chemotherapy
- Novel immune targets:
- LAG-3, TIM-3, TIGIT inhibitors
- Adenosine pathway inhibitors
- Tumor vaccines: Personalized neoantigen approaches
Other Investigational Approaches
- Antibody-drug conjugates: Targeted delivery of cytotoxic agents
- CAR-T cell therapy: Early-phase investigations
- Oncolytic viruses: Engineered to selectively replicate in tumor cells
- Stromal targeting agents: Targeting the dense desmoplastic reaction
The management of cholangiocarcinoma continues to evolve, with increasing emphasis on molecular profiling to guide personalized treatment approaches. While outcomes remain poor overall, advances in surgical techniques, targeted therapies, and multimodal approaches offer hope for improved survival in this challenging malignancy.
9. Prevention & Precautionary Measures
Given the increasing incidence of cholangiocarcinoma worldwide, prevention strategies have gained importance. While complete prevention may not be possible for all risk factors, several strategies can reduce risk or facilitate early detection.
Primary Prevention
Parasite Control in Endemic Areas
- Mass drug administration programs:
- Praziquantel for Opisthorchis viverrini and Clonorchis sinensis
- Periodic community-wide treatment in high-prevalence areas
- Shown to reduce infection prevalence by 50-70%
- Food safety education:
- Avoiding consumption of raw or undercooked freshwater fish
- Proper fish preparation and cooking practices
- Cultural intervention programs in endemic regions
- Sanitation improvements:
- Preventing water contamination with human waste
- Improved sewage systems in endemic communities
- Fish farming practices that reduce parasite exposure
Reduction of Environmental Exposures
- Chemical exposure mitigation:
- Occupational safety measures in high-risk industries
- Personal protective equipment for chemical workers
- Monitoring and regulation of carcinogens like dioxins, nitrosamines
- Water quality improvements:
- Reduction of arsenic and other contaminants in drinking water
- Implementation of water purification systems in high-risk areas
- Food contamination prevention:
- Control of aflatoxin in stored grains
- Limiting nitrosamine formation in preserved foods
- Proper food storage practices
Lifestyle Modifications
- Tobacco cessation:
- Associated with 1.5-2.5 fold risk reduction
- Public health campaigns targeting smoking cessation
- Physician counseling and pharmacotherapy
- Alcohol moderation:
- Limiting intake to moderate levels (≤1 drink/day for women, ≤2 for men)
- Particularly important for patients with underlying liver disease
- Healthy diet:
- Increased consumption of fruits and vegetables
- Reduced intake of preserved/processed foods
- Limited consumption of foods with high nitrosamine content
- Maintenance of healthy weight:
- Weight management programs
- Regular physical activity
- Prevention of metabolic syndrome
Management of Predisposing Conditions
Chronic Liver Disease Control
- Viral hepatitis management:
- Universal hepatitis B vaccination programs
- Screening and treatment of chronic hepatitis B and C
- Antiviral therapy to prevent progression to cirrhosis
- NAFLD/NASH management:
- Weight reduction in overweight/obese patients
- Glycemic control in diabetic patients
- Treatment of dyslipidemia
- Emerging pharmacotherapies for NASH
Primary Sclerosing Cholangitis (PSC) Management
- Ursodeoxycholic acid (UDCA):
- Controversial role in CCA prevention
- May improve biochemical parameters
- No proven survival benefit or reduction in CCA risk
- Management of dominant strictures:
- Endoscopic dilatation
- Short-term stenting when appropriate
- Avoidance of chronic biliary stasis
- Emerging treatments:
- Vancomycin and other antibiotics under investigation
- Antifibrotics in clinical trials
- Gut microbiome modulation strategies
Biliary Tract Disease Management
- Choledochal cyst management:
- Complete excision recommended upon diagnosis
- Even in asymptomatic patients
- 5-year survival >90% with proper management
- Hepatolithiasis treatment:
- Surgical resection of affected segments when feasible
- Stone removal and biliary drainage
- Treatment of underlying causes
- Biliary-enteric anastomosis follow-up:
- Regular monitoring for cholangitis
- Prompt treatment of recurrent infections
- Consideration of surgical revision for chronic problems
Secondary Prevention (Early Detection)
Surveillance in High-Risk Groups
- PSC patients:
- Annual MRCP
- CA 19-9 measurement (with caveats)
- Consideration of ERCP with brushings in selected cases
- Lifelong surveillance recommended
- Liver fluke-endemic area residents:
- Ultrasonography every 6-12 months
- Education about early symptoms
- Stool examination for parasites
- Choledochal cyst/biliary tract abnormality patients:
- Post-surgical surveillance
- Imaging (MRCP or ultrasound) every 1-2 years
- Other high-risk groups:
- Hepatolithiasis: Regular ultrasound
- Post-OLT patients: Routine imaging surveillance
- Lynch syndrome: Consider biliary tract in surveillance programs
Early Symptom Recognition
- Public education campaigns:
- In high-prevalence regions
- Focus on unexplained weight loss, jaundice, pruritus
- Promotion of healthcare seeking for persistent symptoms
- Primary care physician education:
- Recognition of subtle presentation patterns
- Appropriate use of liver function tests
- Timely referral patterns for suspicious findings
Experimental and Developing Approaches
Chemoprevention Strategies
- Aspirin and NSAIDs:
- Promising data from observational studies
- Potential 20-40% risk reduction
- Risk-benefit ratio still under investigation
- Metformin:
- Potential protective effect in diabetic patients
- Mechanism may involve AMPK pathway activation
- Clinical trials ongoing
- Statins:
- Associated with reduced risk in observational studies
- Anti-inflammatory and anti-proliferative effects
- Potential 20-50% risk reduction in some populations
Precision Prevention
- Genetic risk stratification:
- Identification of high-risk genetic variants
- Tailored surveillance for carriers
- Familial risk assessment
- Microbiome modulation:
- Targeting bile acid-microbiome interactions
- Probiotics to reduce inflammation
- Experimental approaches in PSC
Novel Biomarkers for Early Detection
- Liquid biopsy approaches:
- Circulating tumor DNA
- Extracellular vesicles
- Cell-free DNA methylation patterns
- Multi-analyte blood tests:
- Combinations of proteins, metabolites, and genetic markers
- Machine learning algorithms for risk prediction
- Under development and validation
Practical Preventive Recommendations
For the General Population
- Avoid tobacco use
- Limit alcohol consumption
- Maintain healthy weight
- Consume a balanced diet rich in fruits and vegetables
- Avoid raw or undercooked freshwater fish in endemic areas
- Consider hepatitis B vaccination
For Individuals with Risk Factors
- Regular medical follow-up for liver disease
- Prompt investigation of abnormal liver function tests
- Appropriate management of predisposing conditions
- Discussion of surveillance options with healthcare provider
- Consideration of participation in clinical trials of preventive strategies
For Healthcare Providers
- Risk assessment for all patients with liver disease
- Implementation of appropriate surveillance protocols
- Education about modifiable risk factors
- Early investigation of suspicious symptoms
- Multidisciplinary approach to high-risk patients
While cholangiocarcinoma prevention remains challenging, the implementation of comprehensive strategies targeting known risk factors offers the best opportunity to reduce the global burden of this highly lethal malignancy. As understanding of the molecular pathogenesis improves, more targeted preventive approaches may become available.
10. Global & Regional Statistics
Cholangiocarcinoma exhibits remarkable geographical variation in incidence, reflecting different regional risk factor profiles and genetic susceptibilities.
Global Incidence and Prevalence
Overall Incidence
- Global average: 1-2 per 100,000 population annually
- Estimated new cases worldwide: 190,000-220,000 annually
- Trend: Increasing in most regions (3-4% annual increase in Western countries)
- Age-standardized rate: Highest in Eastern Asia, lowest in Africa
- Male:female ratio: Approximately 1.5:1 globally
Geographical Distribution
- Highest incidence regions:
- Northeast Thailand: 85 per 100,000
- Northern China: 10-15 per 100,000
- South Korea: 8-10 per 100,000
- Northern Vietnam: 7-9 per 100,000
- Japan: 3-5 per 100,000
- Intermediate incidence regions:
- Eastern Europe: 2-3 per 100,000
- Southern Europe: 1.5-2.5 per 100,000
- South America (Chile, Argentina): 1.5-3 per 100,000
- Lowest incidence regions:
- North America: 0.5-1.5 per 100,000
- Western Europe: 0.5-1.5 per 100,000
- Australia/New Zealand: 0.5-1 per 100,000
- Sub-Saharan Africa: 0.2-0.5 per 100,000
Intrahepatic vs. Extrahepatic Distribution
- Intrahepatic CCA (iCCA):
- Rising incidence worldwide
- Most dramatic increase in Western countries
- Now constitutes 10-20% of all primary liver cancers
- Extrahepatic CCA (eCCA):
- Relatively stable or slightly decreasing incidence
- Higher proportion in Asia compared to Western countries
- Changing proportions:
- iCCA:eCCA ratio increasing in most countries
- May reflect improved diagnostic classification
Mortality and Survival Rates
Global Mortality
- Annual deaths: Approximately 165,000 worldwide
- Percentage of cancer deaths: 2% of all cancer-related mortality
- Trend: Increasing, particularly for iCCA
- Years of life lost: High due to occurrence in middle age (50-70 years)
Survival Rates by Region
- East Asia:
- 5-year survival: 15-30%
- Higher survival in areas with screening programs
- Earlier stage at diagnosis in endemic regions
- North America:
- 5-year survival: 10-20% overall
- Significant racial disparities (lower in Hispanic and African American populations)
- Improved survival in specialized centers
- Europe:
- 5-year survival: 5-15%
- Better outcomes in Northern Europe
- Significant variation between countries
- Global median survival:
- Untreated: 3-6 months
- With palliative treatment: 6-12 months
- After curative resection: 24-36 months
Survival by Stage
- Stage I: 5-year survival 50% (range 30-60%)
- Stage II: 5-year survival 30% (range 20-40%)
- Stage III: 5-year survival 10% (range 5-15%)
- Stage IV: 5-year survival <5% (median survival 3-6 months)
Factors Influencing Regional Survival Variations
- Healthcare access:
- Timeliness of diagnosis
- Availability of specialized surgical centers
- Access to systemic therapies
- Stage at diagnosis:
- Earlier diagnosis in areas with screening programs
- Improved imaging access
- Treatment differences:
- Varying surgical aggressiveness
- Adoption of novel therapies
- Use of multidisciplinary teams
Country-Wise Comparison and Trends
Thailand
- Incidence: Highest worldwide (85/100,000 in Northeast)
- Risk factors: Predominately O. viverrini infection
- Trend: Gradually decreasing in some areas due to parasite control
- Unique features:
- Earlier median age at diagnosis (50-55 years)
- National screening programs in endemic regions
- High proportion of advanced disease despite awareness
China
- Incidence: Highly variable (1-15/100,000 depending on region)
- Risk factors: C. sinensis infection, hepatolithiasis
- Trend: Increasing in urban areas, stable in rural regions
- Unique features:
- Strong north-south gradient
- Emerging impact of HBV-related CCA
- Increasing recognition of NAFLD-associated cases
Japan
- Incidence: 3-5/100,000
- Risk factors: Hepatolithiasis, PSC, HCV
- Trend: Modest increase over past two decades
- Unique features:
- High proportion of incidental diagnosis
- Aggressive surgical approach
- Extensive use of locoregional therapies
United States
- Incidence: 1.5/100,000 (doubled since 1980)
- Risk factors: Increasing prevalence of NAFLD, obesity, diabetes
- Trend: Continued increase, especially iCCA
- Unique features:
- Notable racial/ethnic disparities
- Higher rates in Native American populations
- Geographic clusters in certain states (Texas, Louisiana)
United Kingdom
- Incidence: 1-2/100,000
- Risk factors: PSC, HCV, obesity
- Trend: Steady increase, particularly iCCA
- Unique features:
- Centralization of hepatobiliary surgery
- National audits of outcomes
- Strong north-south gradient
Italy
- Incidence: 2-3/100,000
- Risk factors: Liver flukes (northern regions), HCV, hepatolithiasis
- Trend: Stabilizing after previous increases
- Unique features:
- High proportion of viral hepatitis-associated CCA
- Strong regional variations
- Pioneer in liver transplantation for CCA
Age and Gender Distribution
Age Patterns
- Global median age: 65 years
- Range by region:
- Southeast Asia: 50-60 years
- Western countries: 65-75 years
- Age-specific incidence:
- Rare before age 40 (<5% of cases)
- Peak incidence in 7th decade
- Increasing incidence with advancing age
Gender Patterns
- Overall ratio: Male predominance (1.2-1.5:1)
- Regional variations:
- Stronger male predominance in high-incidence regions (2:1)
- More equal distribution in low-incidence regions (1.1-1.2:1)
- Subtype differences:
- iCCA: Stronger male predominance
- eCCA: More equal gender distribution
Temporal Trends
Historical Perspective
- 1970s-1980s: Low, stable incidence worldwide
- 1990s-2000s: Beginning of increase, particularly in Western countries
- 2000s-present: Continued rise in most regions
Current Trajectory
- Intrahepatic CCA:
- Annual increase of 2-3% in most developed countries
- Plateauing in some high-incidence Asian regions
- Extrahepatic CCA:
- Stable or slightly decreasing in most regions
- Slight increases in some developing countries
Factors Driving Changes
- Increasing risk factors:
- Obesity, diabetes, NAFLD epidemic
- Aging populations
- Improved survival of patients with chronic liver disease
- Diagnostic improvements:
- Better imaging technologies
- More accurate pathological classification
- Reclassification of some “unknown primary” cancers
- Public health interventions:
- Successful parasite control programs in endemic areas
- Hepatitis vaccination impacts
- Improved management of predisposing conditions
Economic Impact
Healthcare Costs
- Direct annual costs:
- United States: $500-700 million
- Europe: €400-600 million
- Asia-Pacific: $1-1.5 billion
- Per-patient lifetime costs:
- $150,000-300,000 in high-income countries
- Highly variable in middle and low-income regions
- Cost drivers:
- Complex surgical procedures
- Prolonged hospitalizations
- Expensive targeted therapies
- Repeated interventional procedures
Socioeconomic Impact
- Productivity losses:
- Estimated $1-2 billion annually worldwide
- Affects patients primarily during productive years
- Caregiver burden:
- Substantial due to prolonged disease course
- Estimated 20-40 hours weekly for advanced disease
- Regional disparities:
- Catastrophic financial impact in low-resource settings
- Limited access to effective therapies in many regions
The global picture of cholangiocarcinoma epidemiology reflects complex interactions between genetic susceptibility, environmental exposures, and healthcare system factors. The rising incidence in many regions suggests that cholangiocarcinoma will remain a significant global health challenge in the coming decades.
11. Recent Research & Future Prospects
The field of cholangiocarcinoma research has experienced remarkable acceleration in recent years, yielding important insights into disease biology and novel therapeutic approaches.
Recent Advances in Basic Science
Molecular Profiling and Classification
- Comprehensive genomic characterization:
- The Cancer Genome Atlas (TCGA) and International Cancer Genome Consortium (ICGC) studies
- Identification of recurrent genomic alterations (IDH1/2, FGFR2, PRKACA/PRKACB fusions)
- Molecular subtyping into proliferation, inflammation, and metabolism classes
- Integrative multi-omic approaches:
- Combined genomic, transcriptomic, and proteomic analyses
- Epigenomic landscape characterization
- Identification of chromatin remodeling defects in 40-50% of cases
- Single-cell technologies:
- Tumor heterogeneity mapping
- Cell-of-origin studies suggesting distinct progenitor populations
- Detailed characterization of tumor microenvironment components
Tumor Microenvironment Insights
- Immune landscape characterization:
- Generally “cold” immune profile with few tumor-infiltrating lymphocytes
- High proportion of immunosuppressive cells (Tregs, MDSCs)
- Expression of immune checkpoint molecules
- Cancer-associated fibroblasts (CAFs):
- Key role in desmoplastic stroma formation
- Heterogeneous populations with distinct functions
- Emerging therapeutic target
- Tumor-biliary communication:
- Bile acid receptor signaling in carcinogenesis
- Microbiome influences on bile acid metabolism
- Interaction between inflammation and biliary epithelial transformation
Disease Models
- Organoid technology:
- Patient-derived organoids recapitulating tumor characteristics
- Applications in drug screening and personalized medicine
- Biobanking initiatives for rare molecular subtypes
- Genetically engineered mouse models:
- IDH-mutant, KRAS-mutant, and FGFR2-fusion models
- Inflammation-driven models mimicking human disease
- Combination with liver fluke infection for Asian-type CCA
- Novel in vitro systems:
- 3D bioprinting of tumor microenvironment
- Microphysiological systems (“liver-on-a-chip”)
- Co-culture systems with immune components
Clinical Research Advances
Targeted Therapies
- FGFR inhibitors:
- Pemigatinib FDA approval (2020) – first targeted therapy for CCA
- Infigratinib and futibatinib following with similar efficacy
- Development of next-generation inhibitors with improved toxicity profiles
- Resistance mechanisms under investigation
- IDH inhibitors:
- Ivosidenib showing modest but significant benefit
- Combination strategies with chemotherapy and immunotherapy
- Exploration of synthetic lethal approaches
- Other molecular targets:
- BRAF inhibitors for BRAF-mutant cases
- Her2-directed therapies for amplified/overexpressed cases
- TRK inhibitors for NTRK fusion-positive tumors
Immunotherapy Developments
- Checkpoint inhibitor monotherapy:
- Limited efficacy in unselected patients (ORR 5-10%)
- Significant benefit in MSI-high/dMMR subset (ORR 40-50%)
- PD-L1 expression not reliably predictive
- Combination strategies:
- Chemotherapy + immunotherapy trials (ongoing)
- Dual checkpoint blockade (anti-PD-1 + anti-CTLA-4)
- Targeted therapy + immunotherapy combinations
- Novel immune approaches:
- Tumor vaccines (neoantigen, peptide-based)
- CAR-T cell therapies in early development
- Bispecific T-cell engagers
- Oncolytic virotherapy
Biomarker Research
- Liquid biopsy advances:
- ctDNA for molecular profiling and response monitoring
- Early detection signatures under development
- Prediction of recurrence after resection
- Predictive biomarkers:
- Genetic alterations predicting treatment response
- Immune signatures for immunotherapy benefit
- Metabolic profiles for treatment selection
- Novel imaging approaches:
- Radiomics and artificial intelligence applications
- Novel PET tracers (e.g., FGFR-targeted, IDH-targeted)
- Functional MRI techniques
Emerging Therapeutic Strategies
Novel Systemic Approaches
- Antibody-drug conjugates (ADCs):
- Targeting mesothelin, claudin-18.2, other surface proteins
- Enhanced delivery of cytotoxic payloads
- Early clinical trials showing promising signals
- Epigenetic modifiers:
- HDAC inhibitors in combination regimens
- BET inhibitors targeting epigenetic dependencies
- DNA methyltransferase inhibitors
- Cell cycle inhibitors:
- CDK4/6 inhibitors for specific molecular subtypes
- WEE1 inhibitors exploiting DNA damage response defects
- ATR inhibitors in combination strategies
Locoregional Innovation
- Novel radiation approaches:
- FLASH radiotherapy (ultra-high dose rate)
- Proton and carbon ion therapy
- Combination with radiosensitizers
- Interventional radiology advances:
- Development of biodegradable biliary stents
- Drug-eluting beads for TACE
- Irreversible electroporation
- Intraductal therapies:
- Photodynamic therapy refinements
- Radiofrequency ablation of biliary strictures
- Localized drug delivery systems
Surgical Frontiers
- Minimally invasive approaches:
- Robotic complex hepatectomy
- Laparoscopic biliary reconstruction
- Improved perioperative outcomes
- Enhanced preoperative planning:
- 3D printing for surgical navigation
- Virtual reality for procedure planning
- AI-assisted resectability assessment
- Novel transplant protocols:
- Expanded criteria for transplantation in CCA
- Living donor options for hilar CCA
- Machine perfusion techniques to expand donor pool
Future Research Directions
Prevention and Early Detection
- Chemoprevention strategies:
- Clinical trials of aspirin, statins, metformin in high-risk groups
- Development of targeted preventive agents
- Microbiome modulation approaches
- Early detection biomarkers:
- Multi-analyte blood tests
- Bile and urine biomarker panels
- Machine learning algorithms for risk prediction
- Screening protocol development:
- Risk-stratified approaches
- Novel imaging techniques
- Cost-effectiveness analyses in different populations
Precision Oncology Applications
- Comprehensive molecular profiling:
- Moving toward routine testing for all patients
- Expanded panels beyond current actionable alterations
- Integration with clinical and radiographic features
- Novel clinical trial designs:
- Basket and umbrella trials for rare molecular subtypes
- Adaptive designs with biomarker-directed randomization
- Platform trials for efficient therapy evaluation
- Digital pathology and AI:
- Automated diagnostic algorithms
- Prognostic pattern recognition
- Integration with molecular data
International Collaborative Efforts
- Global databases and biorepositories:
- The Cholangiocarcinoma Genomic Consortium
- International harmonization of pathological classification
- Sharing of rare subtype samples and data
- Multi-institutional clinical trials:
- Acceleration of drug development for rare targets
- Standardization of endpoints and response assessment
- Patient-reported outcome incorporation
- Public-private partnerships:
- Industry collaboration for drug development
- Foundation-sponsored research programs
- Patient advocacy group engagement
The pace of discovery in cholangiocarcinoma research has accelerated dramatically, offering new hope for improved outcomes in this challenging malignancy. The transition toward molecularly-guided personalized therapy represents a paradigm shift with potential to significantly impact survival. Integration of these advances into clinical practice, alongside continued investment in basic and translational research, will be essential to maintain momentum in addressing this increasingly recognized global health challenge.
12. Interesting Facts & Lesser-Known Insights
Beyond the clinical and scientific aspects of cholangiocarcinoma lie fascinating insights, historical perspectives, and cultural connections that provide a broader understanding of this complex disease.
Historical Perspectives
Ancient Recognition
- Traditional medicine references: Descriptions of jaundice with liver masses date back to ancient Chinese and Egyptian medical texts (circa 2000 BCE)
- Anatomical understanding: Galen (129-210 CE) described bile ducts but had limited understanding of their pathology
- Early surgical attempts: First documented biliary surgery by John Stough Bobbs in 1867, predating formal recognition of cholangiocarcinoma
Historical Outbreaks
- “Yellow disease epidemics”: Historical records from Thailand describe periodic outbreaks of what was likely fluke-associated cholangiocarcinoma
- Thorotrast legacy: Significant increase in cases 20-30 years after use of Thorotrast (thorium dioxide contrast agent) in the 1930s-1950s
- Occupational clusters: Early industrial clusters in dye, rubber, and chemical workers led to recognition of chemical carcinogenesis
Notable Cases
- Walter Payton: NFL star who died of cholangiocarcinoma in 1999, raising awareness
- Nelson Rockefeller’s youngest son: Death prompted funding for research initiatives
- Emperor Hirohito of Japan: Survived for several months with advanced disease in 1988-1989
- Steve Jobs: Initially misdiagnosed with cholangiocarcinoma before confirmation of neuroendocrine tumor
Unusual Scientific Findings
Geographical Anomalies
- “Cholangiocarcinoma belt”: The geographic band across Southeast Asia with extreme incidence variations within short distances
- “Cancer villages”: Specific communities in China with 20-50 times national average rates, linked to industrial pollution
- North-South European gradient: Unexplained higher rates in Scandinavia compared to Mediterranean countries, despite lower parasite prevalence
Biological Peculiarities
- Microbiome signatures: Distinct bacterial profiles in bile of cholangiocarcinoma patients
- Circadian rhythm effects: Higher risk associated with shift work and circadian disruption
- Viral integration: Evidence of HBV DNA integration into tumor genome, suggesting direct oncogenic mechanism
- Mitochondrial DNA alterations: High frequency of mitochondrial genome changes compared to other cancers
Unexpected Associations
- Inverse relationship with altitude: Lower incidence at higher elevations, possibly related to radiation exposure or oxygen tension
- Reproductive factors: Possible protective effect of multiple pregnancies in some populations
- Psychological factors: Some evidence for stress-induced immune suppression influencing progression
- Solar radiation link: Inverse correlation with UV exposure, suggesting potential vitamin D involvement
Misconceptions vs. Medical Facts
Common Myths
- “Cholangiocarcinoma is always fatal”: While prognosis is poor, 5-year survival exceeds 50% for early-stage disease
- “It only affects elderly patients”: While median age is 65+, cases occur in 30s-40s, especially with PSC or liver fluke exposure
- “Liver transplant is never an option”: Highly selected patients achieve excellent outcomes under established protocols
- “All cases are associated with gallstones”: Most cases have no gallstone relationship; confusion with gallbladder cancer
- “Eastern and Western disease are identical”: Significant biological and etiological differences exist
Misunderstood Aspects
- Diagnostic timing impact: Common misconception that earlier diagnosis always improves outcomes; true for some subtypes but not all
- Inflammation duality: Both tumor-promoting and tumor-inhibiting effects of inflammation, context-dependent
- Screening effectiveness: Limited evidence that general population screening improves outcomes, despite intuitive appeal
- Symptom variation: Wide range of presentations beyond the classic obstructive jaundice
- Treatment response heterogeneity: Same treatment yields dramatically different outcomes in seemingly similar patients
Cultural Connections
Regional Perspectives
- Northeast Thailand: “The cancer in the water” – deep cultural understanding of connection between fish consumption and disease
- Traditional healing approaches: Use of specific herbs for jaundice in regions with high cholangiocarcinoma prevalence
- Spiritual aspects: Buddhist temples in Thailand providing hospice care specifically for cholangiocarcinoma patients
- Community adaptation: Generational knowledge in endemic regions influencing food practices and medical seeking behavior
Impact on Specific Communities
- Fishing communities: Dramatic economic and social impacts in Southeast Asian regions where raw fish consumption was cultural cornerstone
- Indigenous populations: Higher rates among certain Native American tribes, possibly linked to genetic factors or environmental exposures
- Chemical workers: Historical occupational cohorts led to workplace safety reforms
- Medical communities: Development of specialized cholangiocarcinoma centers and physician expertise networks
Surprising Research Developments
Unexpected Therapeutic Avenues
- Anthelmintics as treatment: Drugs designed to kill liver flukes showing direct anti-tumor effects
- Diabetes medications: Metformin demonstrating unexpected anti-cholangiocarcinoma properties
- Psychotropic drugs: Certain antidepressants and antipsychotics with anti-proliferative effects in preclinical models
- Viral therapy: Oncolytic viruses showing particular affinity for cholangiocarcinoma cells
Research Challenges
- Tumor heterogeneity: Single tumors containing multiple distinct genetic subclones
- Micrometastatic disease: Presence of cancer cells outside primary tumor in nearly 90% of seemingly localized cases
- Chemoresistance mechanisms: Unique metabolic adaptations allowing survival in harsh bile environment
- Model difficulties: Historical challenges in developing laboratory models that accurately reflect human disease
Emerging Fields
- Artificial intelligence applications: Machine learning algorithms outperforming radiologists for certain aspects of detection
- Quantitative histopathology: Digital analysis of tumor architecture predicting outcomes better than conventional staging
- Extracellular vesicle research: Tumor-derived exosomes as biomarkers and therapeutic targets
- Microbiome modulation: Targeting bacterial communities in bile to slow progression
Patients and Advocacy
Patient Perspective Insights
- Diagnostic journey: Average of 3-5 doctor visits before diagnosis, with frequent initial misdiagnosis
- Symptom burden: Pruritus often rated as more debilitating than pain by many patients
- Information gaps: Significant disparities in patient understanding between specialized centers and community practice
- Decision-making challenges: Complex treatment decisions with limited evidence creates substantial anxiety
Advocacy Impact
- Cholangiocarcinoma Foundation: Founded in 2006, now coordinates international research efforts
- Rare Cancer Networks: Collaboration among rare cancer organizations amplifying research funding
- Patient-driven research: Significant contributions from patient advocacy to clinical trial design
- Research funding growth: 500% increase in dedicated research funding over past decade
Future Horizons
Emerging Technologies
- Liquid biopsy evolution: Moving toward early detection and recurrence monitoring
- Nanomedicine applications: Bile-resistant nanoparticle delivery systems for targeted therapy
- Biodegradable stents: Self-expanding, drug-eluting biliary stents with programmable degradation
- Molecular imaging: Receptor-specific tracers for early detection and treatment monitoring
Paradigm Shifts
- Reclassification proposals: Moving from anatomical to molecular classification
- Preventive approaches: Shift from treatment to prevention in high-risk regions
- Curative intent expansion: Moving beyond traditional resectability criteria
- Global collaboration models: International databases and tissue repositories
These fascinating aspects of cholangiocarcinoma highlight the complex interplay between biology, environment, culture, and medical science. Understanding these broader perspectives enhances appreciation of the unique challenges and opportunities in addressing this rare but increasingly recognized malignancy.