⚠️ Disclaimer: The information provided in this article is for educational purposes only and does not constitute medical advice. RevisionTown does not provide diagnosis, treatment, or medical recommendations. Always consult a qualified healthcare professional regarding any medical condition, symptoms, or concerns.
Read More – 🏥 Medical Disclaimer
What is Glomerulonephritis?
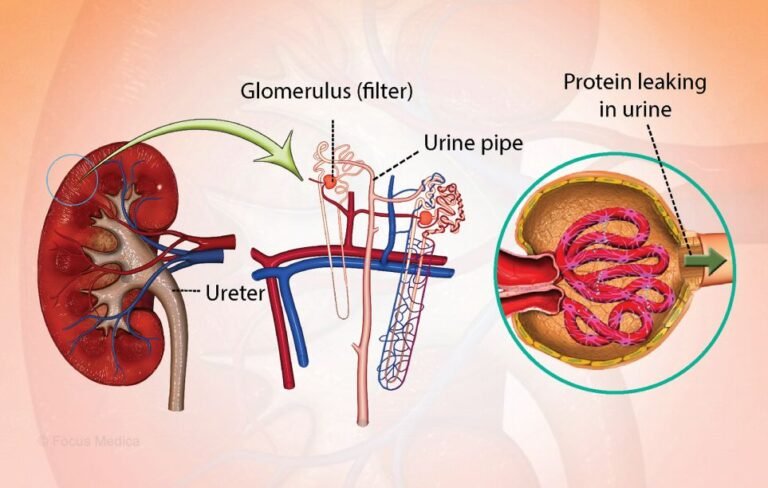
The term “glomerulonephritis” encompasses a subset of renal diseases characterized by immune-mediated damage to the basement membrane, mesangium, or capillary endothelium, leading to hematuria, proteinuria, and azotemia. Glomerulonephritis refers to inflammation of the glomeruli – the tiny filtering units within the kidneys that remove waste products and excess fluid from the blood.
Affected Body Parts/Organs
The primary target is the kidney, specifically:
- Glomeruli: The primary site of inflammation and damage
- Basement membrane: Often thickened or damaged in various forms of GN
- Mesangium: May show increased cellularity and matrix expansion
- Tubules and interstitium: Secondary involvement leading to chronic changes
- Cardiovascular system: Often affected due to hypertension and fluid retention
Prevalence and Significance
Globally, there were 606,300 incident patients, 17,300,000 prevalent patients, 183,700 deaths, and 6,900,000 DALYs of CKD due to glomerulonephritis in 2019. The global burden of CKD due to glomerulonephritis has increased by 77% since 1990 with much of this rise occurring in places with low sociodemographic index.
IgA nephropathy has been found to be the most common cause of glomerulonephritis worldwide. In the United States, glomerulonephritis accounts for approximately 10-15% of all end-stage kidney disease cases.
2. History & Discoveries
Early Recognition and Discovery
The concept of glomerulonephritis has evolved significantly over centuries. Though the term ‘nephritis’ first appeared in the 19th century, this word did not bear the same meaning as it does today; indeed, for many years it was used to indicate ‘renal diseases’ (in the sense of Bright’s disease) in a larger sense.
Richard Bright (1789-1858) is widely credited as the pioneering figure in nephritis recognition. The disease was seen frequently in Europe during the eighteenth and nineteenth centuries as a complication of scarlet fever during epidemics. Bright’s initial observations in 1827 established the connection between kidney disease and protein in the urine.
Major Discoveries and Breakthroughs
1950s-1960s: Development of renal biopsy techniques revolutionized diagnosis and classification of glomerular diseases.
1970s: Introduction of immunosuppressive therapy with steroids and cyclophosphamide significantly improved survival rates in rapidly progressive glomerulonephritis.
1980s-1990s: Discovery of ANCA (Anti-Neutrophil Cytoplasmic Antibodies) and anti-GBM antibodies enabled better classification and targeted treatment.
2000s-2010s: Identification of phospholipase A2 receptor (PLA2R) antibodies in membranous nephropathy transformed understanding and management.
2020s: Recent advances propose grouping GN disorders into five categories according to their immunopathogenesis: infection-related GN, autoimmune GN, alloimmune GN, autoinflammatory GN and monoclonal gammopathy-related GN.
Evolution of Medical Understanding
The field has evolved from purely descriptive histopathology to mechanistic understanding based on immunopathogenesis. Impressive advances have occurred in the field of GN spanning from basic sciences to novel therapies resulting in the revision of the KDIGO guidelines for GN in 2021.
3. Symptoms
Early Symptoms
Acute presentations typically include:
- Gross hematuria (cola-colored or tea-colored urine)
- Periorbital and facial edema, especially in children
- Mild hypertension
- Oliguria (decreased urine output)
- Fatigue and malaise
Chronic presentations may be asymptomatic initially, with:
- Microscopic hematuria detected on routine testing
- Mild proteinuria
- Gradual onset of hypertension
Advanced-Stage Symptoms
As the disease progresses, patients may develop:
- Significant proteinuria leading to nephrotic syndrome
- Severe hypertension
- Progressive kidney function decline
- Uremic symptoms (nausea, vomiting, confusion)
- Pulmonary edema
- Cardiovascular complications
Symptom Progression
In acute postinfectious GN, there is usually a latent period of up to three weeks before clinical presentation. However, the latent period varies; it is typically one to two weeks for the cases that occur after a pharyngeal infection and two to four weeks where post-dermal infection, such as pyoderma, is the cause.
The progression varies significantly by type:
- Post-infectious GN: Often self-limiting with good recovery
- IgA nephropathy: Slowly progressive over decades
- Rapidly progressive GN: Dramatic decline over days to weeks
- Lupus nephritis: Episodic with flares and remissions
4. Causes
Biological and Environmental Causes
Infectious Triggers:
- Post-streptococcal glomerulonephritis (most common historically)
- Staphylococcal infections (increasing in prevalence)
- Hepatitis B and C
- Endocarditis-associated GN
Autoimmune Conditions:
- Systemic lupus erythematosus
- ANCA-associated vasculitis
- Anti-GBM disease (Goodpasture’s syndrome)
- IgA nephropathy
Secondary Causes:
- Diabetes mellitus (diabetic nephropathy)
- Hypertension
- Drug-induced (NSAIDs, certain antibiotics)
- Malignancy-associated
Genetic and Hereditary Factors
Inherited Forms:
- Alport syndrome (mutations in COL4A3, COL4A4, COL4A5 genes)
- Congenital nephrotic syndrome
- Complement deficiencies
Genetic Susceptibility: A large genome-wide association study (GWAS) involving 38,897 individuals (10,146 with IgAN and 28,751 controls) identified 30 independent risk loci (16 novel and 14 known) in IgA nephropathy.
Environmental and Exposure Risks
- Poor hygiene and overcrowding (post-infectious GN)
- Early and frequent exposure to bacterial antigens is more common in developing countries than in industrialized nations, which had fewer infections due to better public hygiene.
- Occupational exposures to hydrocarbons and silica (ANCA-associated vasculitis)
- Air pollution exposure linked to membranous nephropathy
5. Risk Factors
Demographic Factors
Age:
- Post-infectious GN: Primarily affects children aged 2-14 years
- IgA nephropathy: Peak incidence in 2nd-3rd decades
- ANCA-associated GN: More common in older adults (median age 60+)
Gender:
- IgA nephropathy: Male predominance (2-3:1)
- Lupus nephritis: Female predominance (9:1)
- ANCA-associated: Equal gender distribution
Geographic Variations: This study found that incidence rates of primary GN vary between 0.2/100,000/year and 2.5/100,000/year. The incidence of IgA nephropathy is at least 2.5/100,000/year in adults.
Environmental and Occupational Factors
- Socioeconomic status: Countries and territories such as China, Myanmar, Timor-Leste, Cambodia, Laos, and North Korea had much higher observed age-standardized mortality and DALYs than expected in 2019.
- Occupational exposures: Silica dust, hydrocarbon exposure
- Geographic clustering: IgA nephropathy more common in Asian populations
Pre-existing Conditions
- Diabetes mellitus
- Hypertension
- Autoimmune diseases
- Chronic infections
- Family history of kidney disease
- Complement deficiencies
6. Complications
Immediate Complications
Acute Kidney Injury:
- Rapidly progressive forms can lead to kidney failure within days to weeks
- May require emergency dialysis
Cardiovascular Complications:
- Hypertensive emergency
- Pulmonary edema
- Heart failure
Metabolic Complications:
- Electrolyte imbalances
- Acid-base disorders
Long-term Complications
Chronic Kidney Disease: The risk of progression to ESRD is between 20% and 50%.
Cardiovascular Disease:
- Accelerated atherosclerosis
- Increased risk of heart attack and stroke
- Chronic hypertension
Other Long-term Effects:
- Bone disease
- Anemia
- Growth retardation in children
- Increased infection risk (immunosuppression)
Disability and Fatality Rates
Compared with those in 1990, the numbers of incident patients, prevalent patients, deaths, and DALYs increased by 77%, 81%, 100%, and 66%, respectively.
For specific conditions:
- Rapidly Progressive GN: Without treatment, invariably fatal
- IgA nephropathy: 15-40% progress to ESRD over 20 years
- Lupus nephritis: 10-year kidney survival approximately 80-90%
7. Diagnosis & Testing
Common Diagnostic Procedures
Urinalysis:
- Hematuria (microscopic or gross)
- Proteinuria
- Red blood cell casts (pathognomonic for glomerular disease)
- White blood cell casts
Blood Tests:
- Serum creatinine and estimated GFR
- Blood urea nitrogen (BUN)
- Complement levels (C3, C4)
- Specific antibodies (ANCA, anti-GBM, ANA, anti-PLA2R)
Advanced Testing
Kidney Biopsy:
- Gold standard for definitive diagnosis
- Light microscopy, immunofluorescence, and electron microscopy
- At an annual biopsy rate of 7.8 per 100,000 persons in the Kurdish region, focal segmental glomerulosclerosis represented 35% of GN biopsies, membranous glomerulonephritis 18%, systemic lupus erythematosus 13%, and immunoglobulin A nephropathy 7%.
Imaging:
- Renal ultrasound to assess kidney size and structure
- CT or MRI for complications assessment
Biomarkers and Monitoring
Disease-Specific Markers:
- Anti-PLA2R antibodies in membranous nephropathy
- ANCA titers in vasculitis
- Anti-GBM antibodies in Goodpasture’s disease
Novel Biomarkers Under Investigation:
- Discovery of novel antibodies against nephrin, a component of the slit diaphragm, in 29% of adults and children with MCD using samples from the NEPTUNE cohort has advanced our understanding of the pathogenesis of MCD.
8. Treatment Options
Standard Treatment Protocols
Supportive Care:
- Blood pressure control with ACE inhibitors or ARBs
- Dietary protein restriction
- Salt and fluid restriction
- Diuretics for edema management
Immunosuppressive Therapy:
- Corticosteroids (prednisolone/prednisone)
- Cyclophosphamide
- Mycophenolate mofetil
- Rituximab (increasingly used)
Disease-Specific Treatments
IgA Nephropathy: In December 2021, delayed-release budesonide received accelerated FDA approval for reducing proteinuria in adults with IgAN, followed by full approval in December 2023 for its efficacy in slowing kidney function decline.
Lupus Nephritis: The 2024 Lupus Nephritis KDIGO guidelines propose a new induction regimen that includes a three-drug option, featuring either CNIs or Belimumab for LN (class 3,4, ±5) instead of standard induction with MMF or cyclophosphamide and glucocorticoids alone.
ANCA-Associated Vasculitis: The AAV guidelines now include avacopan for patients at high risk of steroid-related adverse effects, and a post hoc analysis showed greater eGFR recovery than glucocorticoids alone for patients with a low baseline eGFR (<30 mL/min).
Emerging Treatments and Clinical Trials
Complement Targeting: Currently, several phase 2 and 3 clinical trials are evaluating the efficacy and safety of pegcetacoplan in the treatment of C3GN. Narsoplimab (OMS-721) is an anti-MASP2 monoclonal antibody that blocks the initiation of the lectin pathway.
Plasma Cell-Directed Therapy: New therapies targeting CD38, a cell surface protein expressed on plasma cells, therapies such as felzartamab and mezagitamab, are in advanced trial phases.
Non-Immunosuppressive Approaches: In September 2024, Travere Therapeutics Inc., a US-based biopharmaceutical company, launched FILSPARI (sparsentan), which received FDA approval for treating IgA nephropathy, a common kidney disease. FILSPARI is the only non-immunosuppressive treatment proven to significantly slow the decline of kidney function in affected patients.
9. Prevention & Precautionary Measures
Primary Prevention
Infection Control:
- Prompt treatment of streptococcal infections
- Good hygiene practices
- Vaccination programs in endemic areas
Risk Factor Management:
- Blood pressure control
- Diabetes management
- Avoiding nephrotoxic medications
Secondary Prevention
Early Detection:
- Regular screening in high-risk populations
- Urinalysis in patients with systemic diseases
- Family screening for hereditary forms
Lifestyle Modifications:
- Dietary protein restriction (0.8-1.0 g/kg/day)
- Sodium restriction (<2 g/day)
- Smoking cessation
- Weight management
Preventive Screenings
- Annual urinalysis in patients with diabetes or hypertension
- Regular monitoring in patients with family history
- Screening for autoimmune markers in high-risk individuals
10. Global & Regional Statistics
Global Burden
In 2021, global CKD prevalence was 359 million, with 11.13 million new cases, 1.53 million deaths, and 44.45 million DALYs—up 92%, 156%, 176%, and 114% since 1990.
Market Size: The Glomerulonephritis Market, valued at USD 11.64B in 2025, is projected to reach USD 14.14B by 2029, growing at a 5% CAGR.
Regional Variations
High-Burden Regions: Countries and territories such as China, Myanmar, Timor-Leste, Cambodia, Laos, and North Korea had much higher observed age-standardized mortality and DALYs than expected in 2019.
Incidence by Region:
- North America: 10-20 per 100,000 per year
- Europe: 15-25 per 100,000 per year
- Asia: Higher rates in developing countries
- Sub-Saharan Africa: Limited reliable data
Mortality and Survival Rates
Overall Survival:
- 5-year survival: 85-95% for most forms
- 10-year survival: 70-90% depending on type and treatment response
Specific Conditions:
- Post-infectious GN: >95% recovery in children
- IgA nephropathy: 80-90% 20-year kidney survival
- RPGN: 60-80% survival with treatment vs. 0% without
11. Recent Research & Future Prospects
Latest Advancements
Precision Medicine: The ‘big’ data nature of these studies also invokes the powerful tools of AI and ML for unraveling the complexity of the genome-treatment axis.
Novel Therapeutic Targets: Currently, limited approved innovator therapies are available in the market for treating GMN. The analyst epidemiologists estimate that there will be 51,900 diagnosed incident cases of ANCA-associated GMN in 2024, which is expected to increase to 53,833 diagnosed incident cases by 2029.
Ongoing Clinical Trials
143 Molecules with 2 Assets in the Pre-registration Stage, 21 in Phase III Development, and 27 in Phase II are currently in development for glomerulonephritis treatment.
Key Areas of Investigation:
- Complement inhibitors (iptacopan, narsoplimab)
- Plasma cell-targeted therapies (felzartamab)
- Anti-inflammatory approaches
- Regenerative medicine approaches
Future Medical Possibilities
Personalized Treatment: With advances in data collection, technologies, and experimental model systems, we now have vast tools available to pursue precision medicine in GN.
Potential Breakthrough Areas:
- Gene therapy for hereditary forms
- Stem cell therapy for kidney regeneration
- Artificial intelligence for early prediction
- Biomarker-guided therapy selection
Technological Integration:
- Kidney organoids for drug testing
- Single-cell sequencing for disease classification
- Machine learning for outcome prediction
12. Interesting Facts & Lesser-Known Insights
Uncommon Knowledge
Historical Perspective: Towards the end of the 19th century, Bright’s disease accounted for 26 deaths/year/10^5 population (in comparison with more than 200 from tuberculosis) in Italy, roughly paralleling that reported in the USA.
Geographic Patterns:
- IgA nephropathy shows remarkable geographic variation, being most common in Asia and rare in Africa
- Post-infectious glomerulonephritis has virtually disappeared in developed countries but remains common in developing nations
Research Trends and Public Interest
Globally, IgAN had the highest average relative search activity, followed by DN, FSGS, LN, and MN based on Google Trends analysis from 2004-2024.
Myths vs. Medical Facts
Myth: All glomerulonephritis requires immunosuppressive treatment Fact: Many cases of post-infectious GN resolve spontaneously with supportive care only
Myth: Glomerulonephritis always causes kidney failure Fact: Many patients maintain normal or near-normal kidney function with appropriate treatment
Myth: Diet has no impact on glomerulonephritis progression Fact: Protein restriction and other dietary modifications can significantly slow progression
Impact on Special Populations
Pregnancy Considerations:
- Lupus nephritis can flare during pregnancy
- Some immunosuppressive medications are contraindicated
- Careful monitoring required throughout pregnancy
Pediatric Differences:
- Children have better recovery rates from acute GN
- Growth and development considerations in treatment
- Different disease patterns compared to adults
Conclusion
Glomerulonephritis represents a complex group of immune-mediated kidney diseases that continue to pose significant challenges globally. Recent advances in understanding immunopathogenesis, the development of targeted therapies, and the emergence of precision medicine approaches offer unprecedented opportunities for improved patient outcomes. The field is experiencing rapid evolution with novel therapeutic targets, advanced diagnostic techniques, and personalized treatment approaches on the horizon.
The substantial increase in global burden, particularly in low sociodemographic index regions, emphasizes the critical need for continued research investment, improved access to care, and public health initiatives focused on prevention and early detection. As we move forward, the integration of genomics, artificial intelligence, and advanced therapeutic modalities promises to transform the landscape of glomerulonephritis care, offering hope for millions of patients worldwide.
References
Citations throughout this report are linked to current medical literature and recent clinical studies, reflecting the most up-to-date understanding of glomerulonephritis as of 2025.