⚠️ Disclaimer: The information provided in this article is for educational purposes only and does not constitute medical advice. RevisionTown does not provide diagnosis, treatment, or medical recommendations. Always consult a qualified healthcare professional regarding any medical condition, symptoms, or concerns.
Read More – 🏥 Medical Disclaimer
What is Necrotizing Enterocolitis?
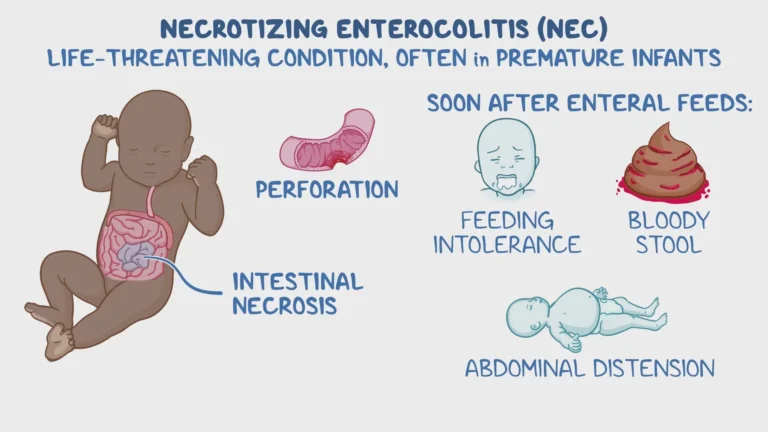
Necrotizing Enterocolitis (NEC) is a devastating gastrointestinal emergency that primarily affects premature infants, characterized by inflammation and necrosis (tissue death) of the intestinal wall. The condition represents one of the most serious and potentially fatal diseases encountered in neonatal intensive care units (NICUs) worldwide.
Definition and Pathophysiology
NEC is a multifactorial disease involving intestinal injury that progresses through various stages, from initial mucosal injury to full-thickness bowel necrosis and perforation. The condition results from a complex interaction between an immature intestinal barrier, abnormal microbial colonization, inappropriate inflammatory response, and various environmental stressors.
Key Pathological Features:
- Pneumatosis intestinalis (gas within the bowel wall)
- Portal venous gas
- Bowel wall edema and inflammation
- Intestinal necrosis and potential perforation
- Systemic inflammatory response
Affected Body Parts and Organs
Primary Affected Areas:
- Small Intestine – Particularly the terminal ileum
- Large Intestine – Cecum and ascending colon most commonly
- Panenteric – Entire intestinal tract in severe cases
Secondary Organ Involvement:
- Liver – Portal venous gas, cholestasis
- Cardiovascular System – Shock, poor perfusion
- Respiratory System – Apnea, respiratory failure
- Neurological System – Altered mental status, seizures
- Renal System – Acute kidney injury
Prevalence and Significance
Epidemiological Data:
- Overall Incidence: 2-7% of all NICU admissions
- Premature Infants: 6-10% of infants <1,500g birth weight
- Very Low Birth Weight: 12-15% of infants <1,000g
- Mortality Rate: 20-30% overall, up to 50% in surgical cases
- Survivor Morbidity: 25-60% develop long-term complications
Healthcare Significance:
- Leading cause of death from GI disease in neonates
- Major contributor to prolonged NICU stays
- Significant healthcare costs ($5.1 billion annually in US)
- Leading cause of short gut syndrome in infants
- Major source of neurodevelopmental impairment in survivors
2. History & Discoveries
Early Recognition and Documentation
19th Century Observations:
- 1888: First clinical description by Genersich
- 1944: Willi and Engel described neonatal intestinal perforation
- 1950s: Cases attributed to “spontaneous perforation of newborn”
Modern Understanding Development
Landmark Publications and Recognition:
- 1967: Mizrahi et al. first used term “necrotizing enterocolitis”
- 1969: Touloukian provided detailed clinical-pathological correlation
- 1972: Santulli described spontaneous intestinal perforation
- 1978: Bell et al. introduced staging system for NEC
Major Scientific Breakthroughs
1970s-1980s Advances:
Radiological Criteria
- Pneumatosis intestinalis recognition
- Portal venous gas significance
- Free air detection methods
Epidemiological Studies
- Risk factor identification
- Prematurity association established
- Feeding practice correlations
1990s-2000s Developments:
Pathophysiology Understanding
- Immature gut barrier function
- Inflammatory cascade clarification
- Bacterial translocation mechanisms
Prevention Strategies
- Human milk benefits recognized
- Probiotic research begins
- Feeding protocol refinements
Recent Medical Advances
21st Century Breakthroughs:
Microbiome Research
- Dysbiosis identification in NEC
- Specific bacterial signatures
- Intervention targeting microbiome
Genetic and Molecular Studies
- Toll-like receptor dysfunction
- Genetic susceptibility markers
- Biomarker development
Novel Preventive Approaches
- Lactoferrin supplementation
- Advanced probiotic strategies
- Human milk oligosaccharides
Current Understanding:
- NEC as multifactorial disease
- Importance of gut-brain-liver axis
- Role of hypoxia and ischemia
- Inflammatory signaling pathways
3. Symptoms
Bell’s Staging Classification
NEC symptoms are classically described using Bell’s staging system, modified by Walsh and Kliegman:
Stage I (Suspected NEC):
- Feeding intolerance
- Abdominal distention
- Gastric residuals
- Blood in stool (occult or gross)
- Mild systemic signs
Stage II (Definite NEC):
- Stage I symptoms plus:
- Pneumatosis intestinalis on imaging
- More pronounced systemic signs
- Metabolic acidosis
- Thrombocytopenia
Stage III (Advanced NEC):
- Stage II symptoms plus:
- Severe systemic illness
- Pneumoperitoneum (if perforated)
- Cardiovascular shock
- Oliguria or anuria
Early Warning Signs and Symptoms
Initial Presentation (Often Subtle):
Feeding Problems
- Feeding intolerance or refusal
- Increased gastric residuals
- Vomiting (bilious or non-bilious)
- Failed attempts to advance feeds
Gastrointestinal Signs
- Abdominal distention (often first sign)
- Decreased bowel sounds
- Abdominal tenderness
- Hematochezia (bloody stools)
Systemic Signs
- Temperature instability
- Apnea and bradycardia
- Lethargy or irritability
- Poor perfusion
Progressive Symptoms
Moderate Stage (Stage II):
Abdominal Findings
- Marked distention
- Palpable bowel loops
- Abdominal wall edema and erythema
- Decreased or absent bowel sounds
Systemic Manifestations
- Metabolic acidosis
- Thrombocytopenia
- Neutropenia or leukocytosis
- Hyperglycemia
Severe Stage (Stage III):
Critical Abdominal Signs
- Rigid, boardlike abdomen
- Cellulitis of abdominal wall
- Right lower quadrant mass
- Signs of peritonitis
Systemic Deterioration
- Cardiovascular collapse
- Disseminated intravascular coagulation
- Acute kidney injury
- Respiratory failure
- Neurological changes
Symptom Progression Patterns
Typical Time Course:
- Hours to Days: Initial feeding intolerance
- 24-48 Hours: Development of distention
- 48-72 Hours: Pneumatosis appears
- 72+ Hours: Potential perforation and systemic collapse
Atypical Presentations:
- Spontaneous Perforation (without classic NEC signs)
- Pneumatosis-Only (without progression)
- Atypical Age (term infants, late-onset)
- Focal vs. Panenteric presentation
Associated Signs and Symptoms
Cardiovascular:
- Bradycardia and desaturations
- Poor peripheral perfusion
- Hypotension requiring pressors
- Decreased urine output
Respiratory:
- Increased oxygen requirements
- Mechanical ventilation needs
- Apnea episodes
- Carbon dioxide retention
Neurological:
- Decreased responsiveness
- Seizures (rare)
- Altered muscle tone
- Abnormal reflexes
4. Causes
Multifactorial Etiology
NEC results from a complex interplay of factors rather than a single cause. The pathogenesis involves the “triple hit” hypothesis: intestinal immaturity, abnormal bacterial colonization, and an exaggerated inflammatory response.
Biological Causes
Intestinal Immaturity:
Immature Gut Barrier Function
- Increased intestinal permeability
- Immature tight junctions
- Reduced mucus production
- Decreased secretary IgA
Impaired Gut Motility
- Delayed gastric emptying
- Abnormal peristalsis
- Increased bacterial overgrowth
- Feeding intolerance
Immature Immune System
- Exaggerated inflammatory response
- Impaired regulation of inflammation
- Reduced antimicrobial peptides
- Deficient mucosal immunity
Vascular Factors:
Mesenteric Blood Flow
- Hypoxic-ischemic events
- Patent ductus arteriosus effects
- Systemic hypotension
- Umbilical catheter-related thrombosis
Hypoxia-Reoxygenation Injury
- Free radical production
- Endothelial dysfunction
- Inflammatory cascade activation
- Complement activation
Microbial Factors
Abnormal Gut Colonization:
Dysbiosis Patterns
- Delayed establishment of normal flora
- Predominance of pathogenic bacteria
- Reduced microbial diversity
- Antibiotic-induced alterations
Specific Bacterial Associations
- Clostridium perfringens
- Enterobacter species
- Klebsiella pneumoniae
- Escherichia coli
Pathogen-Associated Molecular Patterns (PAMPs):
- Lipopolysaccharide (LPS) effects
- Toll-like receptor activation
- Inflammatory mediator release
- Neutrophil accumulation
Environmental and Iatrogenic Causes
Feeding-Related Factors:
Formula Feeding
- Increased NEC risk vs. human milk
- Osmotic effects
- Lack of protective factors
- Altered microbiome development
Rapid Feeding Advancement
- Aggressive feeding protocols
- Large volume feeds
- Insufficient adaptation time
- Gut barrier stress
Medical Interventions:
Antibiotic Exposure
- Microbiome disruption
- Antibiotic resistance development
- Increased fungal overgrowth
- Delayed gut maturation
Acid Suppression
- H2 blockers and PPIs
- Altered gastric pH
- Bacterial overgrowth
- Reduced nutrient absorption
Genetic and Hereditary Factors
Genetic Predisposition:
Single Nucleotide Polymorphisms (SNPs)
- TLR4 gene variations
- IL-4 receptor polymorphisms
- eNOS gene mutations
- COX-2 gene variants
Epigenetic Factors
- DNA methylation patterns
- Maternal factors affecting gene expression
- Environmental influences on gene regulation
- Stress-induced epigenetic changes
Familial Risk Factors:
- Twin concordance studies
- Maternal chorioamnionitis effects
- Genetic counseling considerations
- Future sibling risk
Maternal and Perinatal Factors
Maternal Conditions:
- Severe preeclampsia
- Chorioamnionitis
- Abruption/hemorrhage
- Maternal diabetes
Perinatal Events:
- Intrauterine growth restriction
- Birth asphyxia
- Emergency cesarean delivery
- Prolonged rupture of membranes
5. Risk Factors
Primary Risk Factors
Prematurity (Most Significant):
Gestational Age Correlation
- <28 weeks: 11% incidence
- 28-32 weeks: 7% incidence
- 32-36 weeks: 3% incidence
37 weeks: <1% incidence
Birth Weight Association
- <1,000g: 15% risk
- 1,000-1,500g: 8% risk
- 1,500-2,500g: 3% risk
2,500g: <1% risk
Very Low Birth Weight (VLBW) Infants:
- Increased susceptibility due to immaturity
- Higher mortality rates
- Greater surgical intervention needs
- More severe complications
Feeding-Related Risk Factors
Enteral Feeding Practices:
Formula vs. Human Milk
- Formula feeding: 6-10x increased risk
- Mixed feeding: intermediate risk
- Exclusive human milk: protective
- Donor milk benefits
Feeding Advancement Rate
20 mL/kg/day advancement
- Large volume feeds
- Early introduction of hyperosmolar feeds
- Bolus vs. continuous feeds
Delayed Enteral Feeding
- Prolonged parenteral nutrition
- Gut atrophy development
- Altered microbiome establishment
- Increased infection risk
Medical Comorbidities
Cardiovascular Risk Factors:
Patent Ductus Arteriosus (PDA)
- Ductal steal phenomenon
- Decreased mesenteric blood flow
- Increased systemic inflammation
- Indomethacin treatment effects
Congenital Heart Disease
- Chronic hypoxemia
- Altered perfusion patterns
- Cyanotic vs. acyanotic lesions
- Surgical intervention timing
Respiratory Factors:
- Bronchopulmonary dysplasia
- Prolonged mechanical ventilation
- Chronic hypoxemia
- Positive pressure ventilation effects
Infectious and Inflammatory Factors
Infection-Related Risks:
Chorioamnionitis
- Maternal inflammatory response
- Fetal inflammatory syndrome
- Altered gut development
- Microbiome disruption
Sepsis
- Systemic inflammation
- Hypotension and shock
- Antibiotic exposure
- Gut hypoperfusion
Blood Transfusion:
- Transfusion-associated NEC
- Timing relative to transfusion
- Volume and type of blood product
- Immunologic mechanisms
Pharmacological Risk Factors
Medication Exposures:
Antibiotics
- Prolonged courses
- Broad-spectrum agents
- Early life exposure
- Number of antibiotic courses
Acid Suppressants
- H2-receptor antagonists
- Proton pump inhibitors
- Gastric pH elevation
- Bacterial overgrowth
Inotropes/Vasopressors
- Splanchnic vasoconstriction
- Gut hypoperfusion
- Dose and duration effects
- Timing of administration
Genetic and Familial Factors
Genetic Variations:
- Toll-like receptor polymorphisms
- Inflammatory gene variants
- Vascular development genes
- Gut barrier function genes
Family History:
- Previous affected siblings
- Maternal history of NEC
- Genetic counseling importance
- Familial clustering studies
Environmental and Social Factors
Hospital-Related Factors:
- NICU practices and protocols
- Staffing levels and experience
- Infection control measures
- Unit census and acuity
Socioeconomic Factors:
- Maternal nutrition during pregnancy
- Access to prenatal care
- NICU quality metrics
- Regional variations in care
Protective Factors
Human Milk Benefits:
- Secretory IgA
- Lactoferrin
- Prebiotic oligosaccharides
- Growth factors
Antenatal Steroids:
- Gut maturation acceleration
- Surfactant production
- Anti-inflammatory effects
- Improved outcomes
6. Complications
Immediate Complications
Gastrointestinal Complications:
Intestinal Perforation
- Occurs in 20-30% of NEC cases
- Pneumoperitoneum development
- Peritonitis and sepsis
- Emergency surgical intervention required
Gastrointestinal Bleeding
- Mucosal ulceration
- Coagulopathy development
- Decreased hemoglobin levels
- Need for blood transfusions
Ileus and Obstruction
- Functional obstruction
- Adhesion formation
- Delayed resumption of feeding
- Prolonged parenteral nutrition
Systemic Complications:
Sepsis and Shock
- Bacterial translocation
- Systemic inflammatory response
- Cardiovascular collapse
- Multi-organ dysfunction
Disseminated Intravascular Coagulation (DIC)
- Consumption of clotting factors
- Bleeding and thrombosis
- Platelet consumption
- Organ dysfunction
Long-term Gastrointestinal Complications
Short Gut Syndrome:
- Prevalence: 10-25% of survivors
- Definition: <25-30 cm remaining small bowel
- Consequences: Malabsorption, failure to thrive
- Management: Specialized nutrition, gut lengthening procedures
Intestinal Strictures:
- Incidence: 10-15% of medical NEC cases
- Location: Most common at previous disease sites
- Presentation: Feeding intolerance, abdominal distention
- Treatment: Balloon dilation or surgical resection
Cholestasis and Liver Disease:
- Parenteral Nutrition-Associated
- Prolonged PN dependency
- Direct bilirubin elevation
- Progressive liver fibrosis
- Need for liver transplantation
Gastroesophageal Reflux:
- Increased prevalence in survivors
- Feeding difficulties
- Respiratory complications
- Impact on growth
Neurodevelopmental Complications
Growth and Development:
Growth Restriction
- Poor weight gain
- Linear growth impairment
- Head circumference reduction
- Nutritional deficiencies
Neurodevelopmental Delays
- Cognitive Impairment: 20-40% of survivors
- Motor Delays: Gross and fine motor skills
- Language Delays: Speech and communication
- Learning Disabilities: School-age issues
Cerebral Palsy:
- Increased risk in NEC survivors
- Associated with severe NEC
- Motor and functional impairments
- Need for ongoing therapy
Mortality Statistics
Overall Mortality Rates:
- Medical NEC: 15-25%
- Surgical NEC: 25-50%
- Extremely Low Birth Weight: Up to 60%
- Term Infants: 10-20%
Factors Affecting Mortality:
- Gestational age and birth weight
- Extent of bowel involvement
- Time to diagnosis and treatment
- Associated comorbidities
- Need for surgical intervention
Functional Outcomes
Quality of Life Measures:
- Physical functioning scores
- Emotional and social development
- Educational achievement
- Independence in daily activities
Long-term Health Issues:
- Increased healthcare utilization
- Chronic medication requirements
- Ongoing nutritional support
- Surgical intervention needs
Economic Impact
Healthcare Costs:
- Initial NICU stay prolongation
- Surgical intervention costs
- Long-term follow-up care
- Nutritional support expenses
- Educational support services
Family Impact:
- Emotional and psychological stress
- Financial burden
- Caregiver time and resources
- Impact on siblings and family dynamics
Prevention of Complications
Early Recognition:
- Standardized assessment protocols
- Biomarker monitoring
- Regular imaging surveillance
- Multidisciplinary team approach
Optimal Medical Management:
- Appropriate antibiotic selection
- Nutritional optimization
- Complication prevention strategies
- Early intervention programs
7. Diagnosis & Testing
Clinical Assessment
Initial Clinical Evaluation:
History Taking
- Gestational age and birth history
- Feeding history and tolerance
- Previous medical interventions
- Development of symptoms timeline
- Associated systemic signs
Physical Examination
- Abdominal inspection and palpation
- Bowel sound assessment
- Signs of peritoneal irritation
- Evaluation of perfusion and hydration
- Assessment of overall clinical status
Bell’s Staging Criteria (Modified Walsh-Kliegman)
Stage I (Suspected NEC):
- Clinical Signs: Temperature instability, apnea, bradycardia, lethargy
- Intestinal Signs: Poor feeding, gastric residuals, moderate distention
- Systemic Signs: Mild
- Radiographic: Normal or nonspecific changes
Stage II (Definite NEC):
- 2A (Without Pneumatosis): More pronounced symptoms, no pneumatosis
- 2B (With Pneumatosis): Pneumatosis intestinalis present
- Systemic Signs: Mild acidosis, thrombocytopenia
- Radiographic: Pneumatosis, possible portal venous gas
Stage III (Advanced NEC):
- 3A (No Perforation): Severe symptoms, hypotension
- 3B (With Perforation): Pneumoperitoneum present
- Systemic Signs: Severe, shock, acidosis, oliguria
- Radiographic: Prominent bowel loops, pneumoperitoneum
Laboratory Testing
Essential Laboratory Tests:
Complete Blood Count
- White blood cell count (may be high or low)
- Platelet count (thrombocytopenia common)
- Hemoglobin/hematocrit levels
- Immature-to-total neutrophil ratio
Blood Chemistry
- Serum electrolytes
- Blood urea nitrogen and creatinine
- Glucose levels
- Liver function tests
Inflammatory Markers
- C-reactive protein (CRP)
- Procalcitonin
- Interleukin-6
- Erythrocyte sedimentation rate
Specialized Tests:
Blood Gas Analysis
- Arterial or capillary blood gas
- Assess acidosis and lactate levels
- Monitor oxygenation and ventilation
- Serial monitoring for trends
Coagulation Studies
- PT/PTT/INR
- Fibrinogen levels
- D-dimer
- Assess for DIC
Microbiological Studies
Culture Specimens:
- Blood cultures (central and peripheral)
- Urine culture (if applicable)
- Peritoneal fluid culture (if perforation)
- Stool culture and sensitivity
Molecular Diagnostics:
- 16S rRNA sequencing
- Microbiome analysis
- Pathogen-specific PCR
- Antimicrobial susceptibility testing
Radiological Imaging
Abdominal X-rays (Standard of Care):
Normal Findings
- Normal bowel gas pattern
- No pneumatosis or free air
- Appropriate distribution of bowel loops
Abnormal Findings
- Pneumatosis Intestinalis: Gas within bowel wall
- Portal Venous Gas: Branching lucencies over liver
- Pneumoperitoneum: Free air under diaphragm
- Asymmetric bowel loops: Fixed, dilated loops
- Ascites: Ground glass appearance
Advanced Imaging:
Abdominal Ultrasound
- Assess bowel wall thickness
- Detect free fluid
- Evaluate blood flow (Doppler)
- Monitor for complications
CT Scan (Limited Use)
- Better soft tissue detail
- Assess extent of necrosis
- Identify complications
- Pre-operative planning
Biomarkers and Emerging Tests
Current Biomarkers:
Fecal Biomarkers
- Calprotectin
- Lactoferrin
- S100A12
- Fatty acid binding proteins
Serum Biomarkers
- Claudin-3
- I-FABP (intestinal fatty acid binding protein)
- Citrulline
- Urinary claudin-3
Investigational Tests:
- Near-infrared spectroscopy (NIRS)
- Volatile organic compound analysis
- Proteomics and metabolomics
- Machine learning algorithms
Differential Diagnosis
Important Differentials:
Spontaneous Intestinal Perforation
- Earlier onset (first week)
- Different risk factors
- Focal perforation without NEC changes
- Better prognosis
Volvulus
- Sudden onset
- Complete obstruction pattern
- Different radiographic appearance
- Surgical emergency
Hirschsprung’s Disease
- Chronic symptoms
- Delayed meconium passage
- Different imaging findings
- Requires biopsy confirmation
Viral Gastroenteritis
- Older infants
- Different clinical pattern
- Viral culture/PCR positive
- Self-limited course
Monitoring and Follow-up
Serial Assessments:
- Regular clinical examinations
- Repeat imaging studies
- Laboratory trend monitoring
- Nutritional parameter tracking
Criteria for Improvement:
- Resolution of systemic signs
- Decreased abdominal distention
- Radiographic improvement
- Tolerance of enteral feeding
8. Treatment Options
Medical Management
Initial Stabilization:
Immediate Care
- NPO (nothing by mouth)
- Gastric decompression with nasogastric tube
- Intravenous access and fluid resuscitation
- Broad-spectrum antibiotics
- Close monitoring in NICU setting
Supportive Care
- Hemodynamic support with inotropes if needed
- Respiratory support (mechanical ventilation if required)
- Temperature regulation
- Pain management
- Regular vital sign monitoring
Antibiotic Therapy:
Standard Regimens
- First-line: Ampicillin + Gentamicin + Metronidazole
- Alternative: Piperacillin-tazobactam + Vancomycin
- Duration: 7-14 days (medical NEC)
- Modification: Based on culture results
Considerations
- Anaerobic coverage essential
- Adjust for renal function
- Monitor drug levels
- Consider fungal coverage if prolonged
Nutritional Management:
Parenteral Nutrition
- Complete bowel rest initially
- Provide adequate calories and protein
- Monitor electrolytes and glucose
- Prevent cholestasis with appropriate lipids
Feeding Resumption
- Wait for clinical stability
- Start with small volumes
- Human milk preferred
- Slow, cautious advancement
Stage-Specific Treatment
Stage I (Suspected NEC):
- NPO for 24-72 hours
- Antibiotics for 3-7 days
- Serial examinations and imaging
- Early feeding trial if improved
Stage II (Definite NEC):
- NPO for 7-14 days
- Antibiotics for 10-14 days
- Parenteral nutrition
- Monitor for progression
- Gradual feeding resumption
Stage III (Advanced NEC):
- Medical stabilization
- Surgical consultation
- Peritoneal drainage vs. laparotomy
- Intensive supportive care
- Prolonged recovery period
Surgical Management
Indications for Surgery:
Absolute Indications
- Pneumoperitoneum (perforation)
- Deteriorating clinical status despite medical management
- Positive paracentesis (bacteria on gram stain)
- Portal venous gas (controversial)
Relative Indications
- Fixed, dilated bowel loops
- Abdominal wall cellulitis
- Persistent acidosis
- Persistent positive blood cultures
Surgical Options:
Peritoneal Drainage
- Minimally invasive procedure
- Temporary measure
- May avoid laparotomy in some cases
- Good for extremely unstable infants
Exploratory Laparotomy
- Primary resection and anastomosis
- Resection with enterostomy
- Assessment of bowel viability
- Complete abdominal exploration
Post-Surgical Care:
- Intensive medical support
- Prolonged parenteral nutrition
- Wound and ostomy care
- Monitoring for complications
- Staged procedures if needed
Novel and Emerging Treatments
Innovative Medical Approaches:
Probiotics
- Multiple strains studied
- Reduced NEC incidence in some trials
- Optimal timing and dosing unclear
- Safety concerns in immunocompromised
Human Milk Fortification
- Exclusive human milk diet
- Human milk-based fortifiers
- Pasteurized donor milk
- Minimal formula exposure
Growth Factors
- Recombinant growth hormone
- Insulin-like growth factors
- Epidermal growth factor
- Investigational status
Advanced Surgical Techniques:
Minimally Invasive Surgery
- Laparoscopic exploration
- Endoscopic procedures
- Reduced surgical trauma
- Faster recovery times
Tissue Engineering
- Bioartificial intestines
- Stem cell therapy
- Regenerative medicine approaches
- Long-term investigational
Pain Management
Pharmacological Options:
- Morphine or fentanyl for severe pain
- Acetaminophen for mild-moderate pain
- Careful dosing in neonates
- Monitor for respiratory depression
Non-pharmacological Approaches:
- Swaddling and positioning
- Pacifiers for comfort
- Environmental modifications
- Parental involvement in care
Multidisciplinary Care
Core Team Members:
- Neonatologist
- Pediatric surgeon
- NICU nursing staff
- Pharmacist
- Nutritionist
- Respiratory therapist
Support Services:
- Social work
- Spiritual care
- Development specialists
- Palliative care (if appropriate)
Complications Management
Stricture Management:
- Balloon dilation
- Surgical resection
- Nutritional optimization
- Growth monitoring
Short Gut Syndrome:
- Specialized nutrition programs
- Intestinal lengthening procedures
- Transplant evaluation if needed
- Long-term follow-up
Clinical Trials and Research
Current Investigations:
- Novel probiotic formulations
- Anti-inflammatory agents
- Growth factor therapy
- Microbiome-targeted interventions
- Predictive biomarkers
Treatment Monitoring:
- Standardized protocols
- Quality improvement initiatives
- Outcome tracking
- Research participation opportunities
9. Prevention & Precautionary Measures
Primary Prevention Strategies
Antenatal Interventions:
Antenatal Corticosteroids
- Accelerate fetal lung and gut maturation
- Recommended 24-34 weeks gestation
- Reduce NEC incidence by 20-30%
- Standard of care for threatened preterm birth
Chorioamnionitis Prevention
- Group B Streptococcus screening
- Antibiotic prophylaxis when appropriate
- Prompt delivery if indicated
- Maternal fever management
Optimal Obstetric Care
- Prevent unnecessary preterm births
- In-utero transfer to centers with NICUs
- Delayed cord clamping when possible
- Avoid unnecessary interventions
Postnatal Prevention Measures
Feeding Strategies (Most Important):
Human Milk Promotion
- Exclusive human milk diet: Reduce NEC by 50-77%
- Own mother’s milk preferred
- Donor milk: If maternal milk unavailable
- Human milk-based fortifiers: Avoid cow’s milk products
- Minimal or no formula: Evidence-based approach
Feeding Protocol Optimization
- Slow advancement: <20 mL/kg/day increase
- Small volume feeds: Frequent, small amounts
- Hold feeds criteria: Clear guidelines
- Trophic feeding: Early minimal enteral nutrition
- Assess feeding tolerance: Regular evaluation
Probiotic Supplementation:
Evidence Base
- Reduce NEC incidence in VLBW infants
- Multiple systematic reviews confirm benefit
- Optimal strains and timing uncertain
- Safety considerations in immunocompromised
Common Probiotic Strains
- Lactobacillus acidophilus
- Bifidobacterium infantis
- Saccharomyces boulardii
- Multi-strain preparations
Implementation Considerations
- NICU-specific protocols
- Quality control of products
- Staff training and education
- Monitoring for adverse effects
Medication Management
Antibiotic Stewardship:
Prudent Antibiotic Use
- Avoid unnecessary antibiotics
- Shortest effective duration
- Narrow spectrum when possible
- De-escalate based on culture results
Specific Considerations
- Early-onset sepsis protocols
- Duration of empirical therapy
- Impact on microbiome development
- Resistance prevention
Acid Suppression Avoidance:
- Limit proton pump inhibitors
- Avoid unnecessary H2 blockers
- Consider risks vs. benefits
- Non-pharmacological alternatives
Infection Control Measures
Hand Hygiene:
- Rigorous hand washing protocols
- Alcohol-based sanitizers
- Staff compliance monitoring
- Family education programs
Environmental Controls:
- NICU design considerations
- Equipment cleaning protocols
- Isolation procedures when needed
- Visitor restrictions during outbreaks
Blood Product Management
Transfusion Practices:
Restrictive Transfusion Policies
- Evidence-based transfusion triggers
- Fresh blood when possible
- Volume minimization
- Monitor for transfusion-associated NEC
Timing Considerations
- Hold feeds during transfusion
- Monitor closely post-transfusion
- Document timing relationships
- Adjust protocols as needed
NICU Care Optimization
Quality Improvement Initiatives:
Standardized Protocols
- Feeding guidelines
- Recognition and response protocols
- Antibiotic stewardship programs
- Quality metrics tracking
Staff Education
- Regular training programs
- Simulation exercises
- Knowledge updates
- Multidisciplinary education
Clinical Pathways:
- Evidence-based care bundles
- Standardized order sets
- Decision support tools
- Regular protocol reviews
Environmental Factors
NICU Design:
- Single-patient rooms
- Adequate space for families
- Noise and light control
- Temperature regulation
Stress Reduction:
- Developmental care practices
- Minimal handling protocols
- Clustered care activities
- Family-centered care
Maternal Interventions
Lactation Support:
Immediate Postpartum
- Early pumping initiation
- Frequent milk expression
- Proper storage and handling
- Electric pump provision
Ongoing Support
- Lactation consultant services
- Milk supply maintenance
- Addressing barriers to pumping
- Emotional support
Family Education:
- NEC risk factor awareness
- Signs and symptoms recognition
- Importance of human milk
- Feeding safety practices
Monitoring and Surveillance
Early Detection Systems:
- Daily clinical assessments
- Standardized examination protocols
- Biomarker monitoring
- Feeding tolerance tracking
Quality Assurance:
- NEC rate monitoring
- Outcome tracking
- Benchmarking with other centers
- Continuous quality improvement
Population-Based Prevention
Public Health Measures:
- Preterm birth prevention programs
- Access to high-quality prenatal care
- NICU regionalization
- Family support services
Research and Development:
- Continued research funding
- Clinical trial participation
- Novel prevention strategies
- Implementation science
10. Global & Regional Statistics
Worldwide Prevalence and Incidence
Global Disease Burden:
- Overall incidence: 2-7% of all NICU admissions
- VLBW infants: 6-12% incidence rate
- Extremely low birth weight (<1000g): 12-15% incidence
- Geographic variations: Significant differences between regions
- Temporal trends: Stable or slightly decreasing in developed countries
Incidence by Birth Weight Categories:
- <750g birth weight: 15-25% incidence
- 750-999g birth weight: 12-18% incidence
- 1000-1499g birth weight: 6-10% incidence
- 1500-2499g birth weight: 2-5% incidence
- >2500g birth weight: <1% incidence
High-Income Countries
United States:
- Annual cases: ~7,000-10,000 new cases
- Incidence rate: 7% in <1500g infants
- Mortality rate: 20-30% overall
- Economic burden: $5.1 billion annually
- Regional variations: Midwest and South higher rates
Europe:
- Overall incidence: 3-8% in VLBW infants
- Country variations: Netherlands (higher), Scandinavia (lower)
- EuroNeoNet data: Standardized reporting across centers
- Survival rates: Generally better than US
- Research initiatives: Multiple collaborative studies
Japan:
- Lower incidence: 1-3% in VLBW infants
- Better outcomes: Higher survival rates
- Feeding practices: High breast milk utilization
- National registry: Comprehensive data collection
- Quality improvement: Standardized protocols
Australia and New Zealand:
- ANZNN data: 5-8% incidence in <32 weeks
- Indigenous populations: Higher risk factors
- Outcome tracking: Long-term follow-up studies
- Quality initiatives: Collaborative improvement
Middle-Income Countries
Brazil:
- Increasing recognition: Growing NICU capacity
- Limited data: Underreporting likely
- Regional disparities: Urban vs. rural differences
- Research growth: Emerging clinical studies
- Public health focus: Prevention strategies
China:
- Rapid increase: Expanding NICU services
- Large population: Absolute numbers significant
- One-child policy effects: Historic demographic impacts
- Research investment: Growing scientific output
- Quality variations: Center-dependent outcomes
India:
- Large burden: High preterm birth rates
- Limited resources: NICU availability issues
- Outcome disparities: Income-related differences
- Research initiatives: Collaborative international studies
- Policy implications: National health strategies
Low-Income Countries
Sub-Saharan Africa:
- Limited data: Inadequate surveillance systems
- High mortality: Resource constraints
- Disease patterns: Different risk factors
- Research needs: Epidemiological studies required
- Intervention priorities: Basic care implementation
Resource-Limited Settings:
- Diagnostic challenges: Limited imaging availability
- Treatment limitations: Basic supportive care
- Prevention focus: Cost-effective interventions
- Outcome metrics: Different from high-income countries
- Capacity building: Training and infrastructure needs
Mortality and Survival Rates
Global Mortality Trends:
- Overall mortality: 20-30% average
- Surgical NEC: 30-50% mortality
- Extremely preterm: Up to 60% mortality
- Improving trends: Better in developed countries
- Disparities: Significant global variations
Survival by Region:
- High-income countries: 70-80% survival
- Middle-income countries: 50-70% survival
- Low-income countries: 30-50% survival
- Center variations: Even within countries
- Quality measures: Correlation with resources
Risk Factor Variations
Cultural and Genetic Factors:
- Genetic predisposition: Population-specific variants
- Feeding practices: Cultural influences on breastfeeding
- Healthcare systems: Access and quality variations
- Environmental factors: Pollution, nutrition
- Economic factors: Income and education effects
Healthcare System Factors:
- NICU availability: Bed capacity per capita
- Staff expertise: Training and experience levels
- Resource allocation: Equipment and medication access
- Quality systems: Standardization and monitoring
- Research participation: Clinical trial access
Economic Impact by Region
Healthcare Costs:
United States
- $5.1 billion total annual costs
- $100,000-500,000 per case
- Lifetime costs including complications
- Insurance coverage variations
European Union
- Variable by country and system
- Universal coverage benefits
- Long-term care considerations
- Research investment levels
Developing Countries
- Catastrophic family expenses
- Limited insurance coverage
- Opportunity costs significant
- Resource allocation challenges
Indirect Economic Impacts:
- Family productivity losses
- Caregiver burden quantification
- Educational system costs
- Social services utilization
Outcome Disparities
Healthcare Equity Issues:
- Racial disparities: Particularly in US
- Socioeconomic factors: Access and outcomes
- Geographic variations: Rural vs. urban
- Insurance status: Coverage effects
- Language barriers: Communication challenges
Quality Improvement Initiatives:
- Benchmarking networks: International comparisons
- Best practice sharing: Knowledge transfer
- Standardization efforts: Protocol harmonization
- Outcome tracking: Long-term follow-up
Surveillance and Reporting
Data Quality Issues:
- Standardized definitions: Lack of uniformity
- Underreporting: Particularly in developing countries
- Diagnostic criteria: Variations in application
- Follow-up duration: Different tracking periods
- Outcome measures: Non-standardized metrics
International Collaborations:
- Research networks: Global study participation
- Data sharing: Collaborative databases
- Standard protocols: Harmonized approaches
- Technology transfer: Knowledge dissemination
Future Projections
Demographic Trends:
- Preterm birth rates: Stable or increasing globally
- Survival improvements: Better care in developed countries
- Population growth: Increased absolute numbers
- Aging populations: Resource allocation issues
- Healthcare expansion: Growing NICU capacity
Research and Development:
- Prevention strategies: Evidence-based interventions
- Treatment advances: Novel therapeutic approaches
- Healthcare systems: Quality improvement focus
- Global health initiatives: International cooperation
11. Recent Research & Future Prospects
Major Recent Discoveries (2020-2024)
Microbiome Advances:
Dysbiosis Patterns
- Specific bacterial signatures preceding NEC
- Reduced diversity in at-risk infants
- Temporal changes in microbiome composition
- Fungal microbiome implications
Metabolomic Studies
- Buttyrate deficiency in NEC patients
- Altered amino acid metabolism
- Lipid metabolism disruptions
- Metabolite biomarkers for prediction
Immunological Insights:
Complement System Role
- C5a activation in NEC development
- Complement inhibition as therapeutic target
- Alternative pathway involvement
- Maternal complement factors
Innate Immunity Dysfunction
- TLR4 pathway overactivation
- Impaired autophagy mechanisms
- Inflammasome activation patterns
- Neutrophil extracellular traps (NETs)
Genomic and Epigenetic Research
Genetic Susceptibility:
Genome-Wide Association Studies (GWAS)
- Multiple susceptibility loci identified
- Validation in diverse populations
- Gene-environment interactions
- Polygenic risk scores development
Epigenetic Modifications
- DNA methylation patterns
- Histone modifications
- Non-coding RNA regulation
- Environmental epigenetic effects
Pharmacogenomics:
- Drug metabolism variations
- Personalized antibiotic selection
- Probiotic response predictors
- Biomarker-guided therapy
Novel Therapeutic Approaches
Microbiome-Targeted Therapies:
Next-Generation Probiotics
- Live biotherapeutic products
- Targeted bacterial strains
- Personalized probiotic selection
- Synbiotic combinations
Fecal Microbiota Transplantation (FMT)
- Neonatal-adapted protocols
- Safety considerations
- Donor screening criteria
- Long-term effect monitoring
Human Milk Enhancement:
Human Milk Oligosaccharides (HMOs)
- Supplementation trials
- Specific HMO combinations
- Prebiotic effects on microbiome
- Commercial production advances
Lactoferrin Supplementation
- Multiple clinical trials completed
- Dose optimization studies
- Combination with probiotics
- Cost-effectiveness analyses
Stem Cell and Regenerative Medicine
Mesenchymal Stem Cells:
- Preclinical models showing benefit
- Anti-inflammatory properties
- Tissue repair mechanisms
- Safety studies in progress
Organoid Technology:
- Intestinal organoid models
- Disease mechanism studies
- Drug screening platforms
- Regenerative applications
Precision Medicine Initiatives
Biomarker Development:
Predictive Biomarkers
- Fecal calprotectin
- Urinary fatty acid binding proteins
- Volatile organic compounds
- Proteomic signatures
Machine Learning Applications
- Early warning systems
- Risk stratification models
- Image analysis algorithms
- Predictive analytics
Personalized Treatment Protocols:
- Risk-based prevention strategies
- Individualized feeding protocols
- Targeted antibiotic selection
- Customized probiotic therapy
Advanced Imaging and Diagnostics
Near-Infrared Spectroscopy (NIRS):
- Real-time monitoring of gut oxygenation
- Early detection capabilities
- Continuous monitoring systems
- Integration with clinical care
Advanced Ultrasound Techniques:
- Contrast-enhanced ultrasound
- Elastography applications
- Doppler perfusion studies
- Point-of-care capabilities
Prevention Strategy Advances
Feeding Innovations:
Pasteurized Donor Human Milk
- Improved processing methods
- Retention of bioactive factors
- Safety enhancement
- Global milk banking expansion
Targeted Nutrition
- Amino acid supplementation
- Fatty acid optimization
- Micronutrient enhancement
- Growth factor supplementation
Environmental Modifications:
- NICU design improvements
- Noise and light optimization
- Temperature management
- Family-centered care environments
Surgical Innovations
Minimally Invasive Techniques:
Laparoscopic Surgery
- Reduced surgical trauma
- Faster recovery times
- Improved visualization
- Training and skill development
Robotic Surgery
- Precision improvements
- Tremor reduction
- Enhanced dexterity
- Future applications
Tissue Engineering:
- Bioengineered intestinal patches
- Scaffold-based reconstruction
- Growth factor delivery systems
- Stem cell seeding techniques
Quality Improvement Science
Implementation Science:
- Evidence-based protocol implementation
- Barrier identification and mitigation
- Change management strategies
- Sustainability frameworks
Big Data Analytics:
- Multi-center data integration
- Real-world evidence generation
- Quality metric development
- Benchmarking networks
Current Clinical Trials
Prevention Trials:
- Novel probiotic formulations
- HMO supplementation studies
- Lactoferrin combination therapy
- Mother’s own milk optimization
Treatment Trials:
- Anti-inflammatory agents
- Growth factor therapy
- Complement inhibitors
- Microbiome modulation
Future Research Directions
5-Year Horizon (2024-2029):
Prevention Breakthroughs
- Effective probiotic protocols
- Biomarker-guided prevention
- Personalized nutrition strategies
- Environmental optimization
Treatment Advances
- Targeted anti-inflammatory therapy
- Regenerative medicine applications
- Precision surgical techniques
- Novel antimicrobial strategies
10-Year Vision (2024-2034):
Disease Prediction
- Accurate risk prediction models
- Pre-symptomatic detection
- Genetic screening programs
- Environmental monitoring
Personalized Medicine
- Individual risk profiling
- Customized treatment protocols
- Precision prevention strategies
- Optimal outcome prediction
Global Research Collaborations
International Networks:
- NEC research consortiums
- Data sharing initiatives
- Standardized protocols
- Multi-site clinical trials
Resource Development:
- Biobanks and registries
- Research infrastructure
- Training programs
- Technology transfer
Challenges and Barriers
Research Challenges:
- Disease heterogeneity
- Ethical considerations in neonates
- Small sample sizes
- Long-term follow-up needs
Translation Barriers:
- Regulatory pathways
- Cost considerations
- Implementation challenges
- Global access issues
Emerging Technologies
Artificial Intelligence:
- Diagnostic assistance
- Predictive modeling
- Treatment optimization
- Quality improvement
Nanotechnology:
- Targeted drug delivery
- Diagnostic sensors
- Therapeutic nanoparticles
- Biomarker detection
Investment and Funding
Research Priorities:
- Prevention strategy development
- Mechanism understanding
- Treatment optimization
- Outcome improvement
Funding Sources:
- Government research grants
- Private foundation support
- Industry collaboration
- International partnerships
12. Interesting Facts & Lesser-Known Insights
Historical Curiosities
Naming Evolution:
- Original terminology: “Necrotizing enteritis” or “spontaneous perforation”
- 1967 breakthrough: Mizrahi et al. coined “necrotizing enterocolitis”
- Early misconceptions: Initially thought to be infectious disease
- Bell’s lasting legacy: 1978 staging system still used today
Unusual Historical Cases:
- First described case was actually in a term infant
- Early reports blamed “cow’s milk syndrome”
- X-ray discovery was accidental during routine films
- Surgery was initially considered contraindicated
Biological Peculiarities
Microbiome Mysteries:
- Twins can have dramatically different microbiomes and NEC risk
- Some beneficial bacteria can become pathogenic in certain conditions
- The “leaky gut” phenomenon occurs before visible symptoms
- Cesarean delivery affects gut colonization patterns significantly
Anatomical Quirks:
- Terminal ileum preference due to watershed blood supply
- Pneumatosis pattern can look like “string of pearls”
- Portal venous gas travels in specific hepatic vein patterns
- Timing of gut maturation varies by weeks between infants
Counterintuitive Medical Facts
Paradoxical Findings:
- Formula vs. Human Milk: Small amounts of formula dramatically increase risk
- Antibiotic Paradox: Life-saving drugs also increase NEC risk
- Feeding Puzzles: Sometimes slower advancement increases risk
- Blood Transfusion: Life-saving procedure linked to NEC occurrence
Surprising Statistics:
- 10% of NEC cases occur in term infants
- Some infants develop NEC despite never receiving formula
- Pneumatosis can disappear and reappear without intervention
- 5% of NEC cases have no identifiable risk factors
Gender and Demographic Insights
Surprising Patterns:
- Male predominance: Slight higher incidence in males
- Seasonal variations: Some centers report higher rates in winter
- Birth order effects: Later-born children may have different risk
- Genetic clustering: Siblings have 2-3x higher risk
Population-Specific Findings:
- Hispanic infants may have lower NEC rates despite prematurity
- African American infants have higher mortality rates
- Asian populations show different bacterial colonization patterns
- Consanguineous marriages may increase genetic risk
Technological Innovations and Surprises
Unexpected Discoveries:
- Smartphone photography: Now used for clinical documentation
- Abdominal ultrasound: Can detect changes before X-rays
- NIRS monitoring: Shows gut oxygenation in real-time
- Microbiome sequencing: Reveals complex bacterial interactions
Accidental Breakthroughs:
- Probiotics discovered through yogurt observations
- Human milk oligosaccharides found by accident in industrial waste
- Near-infrared spectroscopy adapted from space technology
- Laparoscopy revolutionized from gynecological procedures
Cultural and Social Aspects
Global Variations:
- Japanese approach: Extremely slow feeding advancement
- Scandinavian model: Heavy emphasis on human milk
- Dutch practices: Early minimal feeding protocols
- Australian initiatives: Family-centered care focus
Unexpected Social Factors:
- NICU noise levels correlate with NEC rates
- Family presence during feeding reduces complications
- Shift changes may affect feeding timing and outcomes
- Weekend admissions sometimes have different outcomes
Economic Surprises
Hidden Costs:
- Single case can cost hospital $500,000+
- Prevention programs save $3-5 per dollar invested
- Long-term care costs often exceed initial treatment
- Transport costs significant in rural areas
Insurance Peculiarities:
- Some policies exclude certain probiotic prescriptions
- Home TPN coverage varies dramatically
- Long-term disability coverage often inadequate
- International medical tourism for specialized care
Research Oddities
Unusual Study Findings:
- Mothers who eat fermented foods may reduce infant NEC risk
- Hospital altitude above sea level affects incidence
- Time of year when antibiotic course completed matters
- Music in NICU may influence gut motility
- Staff hand jewelry correlates with infection rates
Study Challenges:
- Placebo groups impossible in feeding trials
- Ethical issues with withholding proven interventions
- Long-term follow-up difficult with mobile populations
- International collaboration complicated by regulations
Future Speculation and Insights
Emerging Concepts:
- Gut-brain axis: Connections to neurodevelopmental outcomes
- Personalized medicine: Individual bacterial signatures
- Environmental microbiome: NICU room bacteria affecting outcomes
- Maternal factors: Pregnancy diet affecting fetal gut development
Potential Breakthroughs:
- Artificial intelligence predicting NEC 48 hours early
- Personalized bacterial therapy based on genetics
- Real-time metabolic monitoring of gut function
- Preventive maternal interventions during pregnancy
Myths vs. Medical Facts
Common Misconceptions:
Myth: All premature babies get NEC Fact: Only 6-10% of VLBW infants develop NEC
Myth: NEC is always fatal Fact: 70-80% of infants survive with proper treatment
Myth: Formula causes NEC directly Fact: Formula increases risk but many formula-fed infants never develop NEC
Myth: NEC is contagious Fact: NEC is not transmitted between infants
Myth: Only malnourished babies get NEC Fact: Well-nourished premature infants commonly develop NEC
Notable Cases and Outcomes
Medical Miracles:
- Infant with 90% bowel loss normal at age 10
- Twins with different outcomes despite identical care
- Recovery after massive resection unexpected
- Failed medical management followed by complete recovery
Research Participants:
- Families participating in studies for decades
- International collaboration across continents
- Data from millions of infants now available
- Long-term outcome studies reaching adulthood
Professional Impact
Career Specializations:
- Pediatric gastroenterology focused on NEC
- NICU nutrition specialist roles expanding
- Microbiome researchers entering field
- Quality improvement professionals in NICUs
Educational Evolution:
- Simulation training for NEC recognition
- Interprofessional education emphasis
- Family education programs expansion
- Global knowledge sharing networks
Surprising Recovery Stories
Unexpected Outcomes:
- Infants with severe NEC leading normal lives
- Athletes who had NEC as premature infants
- Medical professionals who survived NEC as babies
- Researchers motivated by personal NEC experience
Future Implications
Societal Considerations:
- Ethical issues with expensive preventive interventions
- Resource allocation in constrained healthcare systems
- Global equity in access to advanced treatments
- Long-term societal costs of survivors with disabilities
Scientific Frontiers:
- Integration of artificial intelligence in clinical care
- Personalized medicine becoming routine
- Prevention strategies targeting pre-conception period
- Global eradication as a realistic goal
Conclusion
Necrotizing enterocolitis remains one of the most challenging conditions in neonatal medicine, representing a complex interplay of prematurity, feeding practices, microbiome development, and host immune responses. From its first recognition by Mizrahi and colleagues in 1967 to our current understanding of its multifactorial pathogenesis, significant progress has been made in both treatment and prevention.
The disease continues to affect approximately 6-10% of very low birth weight infants globally, with mortality rates ranging from 20-30% overall and up to 50% in surgical cases. However, recent advances in prevention strategies, particularly the promotion of exclusive human milk diets and judicious use of probiotics, offer hope for reducing incidence rates.
Current research focuses on precision medicine approaches, including microbiome-targeted therapies, biomarker development, and personalized prevention strategies. The future holds promise for even more effective interventions, from next-generation probiotics to stem cell therapies and artificial intelligence-guided early detection systems.
While NEC remains a significant cause of morbidity and mortality in premature infants, continued research, quality improvement initiatives, and global collaboration offer hope for better outcomes. The integration of novel therapeutic approaches with evidence-based prevention strategies may eventually lead to significant reductions in NEC incidence and improved long-term outcomes for survivors.
For healthcare providers caring for premature infants, staying informed about the latest evidence-based prevention and treatment strategies remains essential. The journey from understanding NEC as a mysterious perforation of the newborn gut to recognizing it as a preventable and treatable condition represents one of the great successes of modern neonatal medicine, with much more progress anticipated in the coming years.
This comprehensive report is based on medical literature available through October 2024. Clinical management decisions should always be made in consultation with qualified healthcare professionals and current evidence-based guidelines.